Abstract
BACKGROUND: Recent advances in imaging and the use of prognostic indices and molecular profiling have improved our ability to characterize disease and predict outcomes in diffuse large B cell lymphoma (DLBCL). About 1/3rd of patients with DLBCL have bone marrow involvement (BMI) at the time of diagnosis, and bone marrow aspirate/biopsy (BMAB) is considered the gold standard to detect such involvement. [18F] fluorodeoxyglucose (FDG) positron emission tomography combined with computed tomography (PET-CT), has become a standard pre-treatment imaging in DLBCL and may be a noninvasive alternative to BMAB to ascertain BMI. Prior studies have suggested that PET-CT scan may obviate the need for BMAB as a component for staging patients with newly diagnosed DLBCL, but owing to a variety of reasons this is not yet a standard of practice. The aim of this retrospective study which included 99 patients with newly diagnosed de-novo DLBCL, who had undergone both BMAB and PET-CT, was to determine the accuracy of PET-CT in detecting BMI in DLBCL and define overall survival (OS) in these patients based on BMI by BMAB vs. PET-CT.
METHODS: This study is a single institution retrospective review of patients' medical records. All patients with newly diagnosed DLBCL at Virginia Mason Medical Center between January 2004 to December 2013 who underwent pretreatment PET-CT and BMAB were included. PET-CT images were visually assessed for BMI including the posterior iliac crest. Patients with primary mediastinal DLBCL, previous history or co-existence of another lymphoma subtype and those with a non-diagnostic BMAB, and in whom the PET-CT did not show marrow signal abnormality were excluded from the analysis. Ann Arbor stage was determined using PET-CT with and without the contribution of BMAB, and the proportion of stage IV cases by each method was measured.
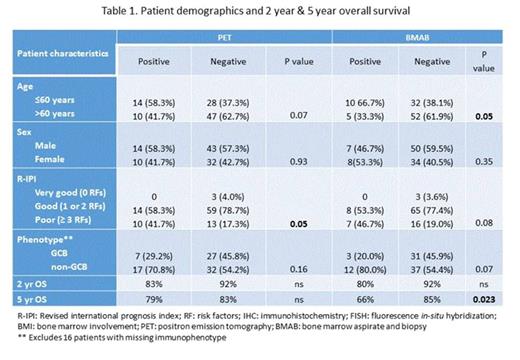
RESULTS: 99 eligible patients were identified. The median age was 62 years (range, 24-88), 62 (59%) were male, 53 (50%) had elevated LDH and 17 (16%) had an ECOG performance status of >2. Thirteen (12%) patients had > 1 extra-nodal site of lymphoma involvement. R-IPI score was 1 in 39 (37%), 2 in 42 (40%), 3 in 20 (19%), and 4 in 4 (4%) patients. A total of 38 (36%) patients had BMI established by either PET-CT (n=24, 19%), BMAB (n=14, 13%), or both (n=12, 11%). 12 of the 24 patients (50%) with positive PET-CT had BMI by DLBCL, while only 2 of the 81 patients (2%) with negative PET-CT showed BMI. BMAB upstaged 1 of the 53 (2%) stage I/II patients to stage IV. The sensitivity of PET-CT scan to detect BMI by DLBCL was 86% while the specificity was 87%. 84 patients (85%) had concordant results between lymphomatous BMAB and PET-CT (12 patients were positive for both, and 72 patients were negative for both), but 15 patients (15%) had a discordant interpretation (3 patients were positive by BMAB and negative by PET-CT, and 12 patients were negative by BMAB and positive by PET-CT). PET-CT was highly accurate for detecting BMI at diagnosis in de-novo DLBCL. Although patients with positive BMAB patients had inferior 5 year OS estimates compared to negative BMAB (66% vs. 85%), no difference was demonstrated between PET-CT positive vs. PET- CT negative patients. (79% vs. 83%) (Table 1)
CONCLUSIONS: In patients with newly diagnosed DLBCL, PET-CT is highly accurate in detecting BMI by lymphoma. In clinical practice, routine BMAB may no longer be necessary for all patients with DLBCL, who are staged by PET-CT, unless the results would change both staging and therapy. The prognostic implication of BMI identified by PET-CT compared to BMAB remains unknown. Whether a PET-CT precludes the need for a BMAB in patients with DLBCL remains to be evaluated in a prospective study.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.