Abstract
Objectives: Compare the outcomes of allogeneic stem cell transplantation (allo-HSCT) versus a combination of imatinib and chemotherapy in patients with Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ALL). Explore prognostic factors and indentify those who may enjoy long-term survival without the risk of allo-HSCT.
Methods: Between May 2006 to November 2015, data of consecutive newly-diagnosed Ph+ALL patients <65 years treated at Peking University People's Hospital were analyzed retrospectively. Patients received imatinib 400mg daily plus CODP regimen as induction chemotherapy. After achieving a complete remission (CR), they received imatinib with 8 cycles of alternating reduced-intensity hyper-CVAD regimen as consolidation chemotherapy. Patients in CR continued maintenance imatinib, vincristine, and prednisone for 2 years, which was followed by imatinib indefinitely. Patients eligible for allo-HSCT underwent it based on their own choice after at least 2 cycles of consolidation regimen during their first CR. Minimal residual disease (MRD) for BCR-ABL by quantitative polymerase chain reaction was monitored after each cycle of induction and consolidation chemotherapy and every 3 months later. Dasatinib was used as the second-line tyrosine kinase inhibitors (TKI) once imatinib-resistance occurred.
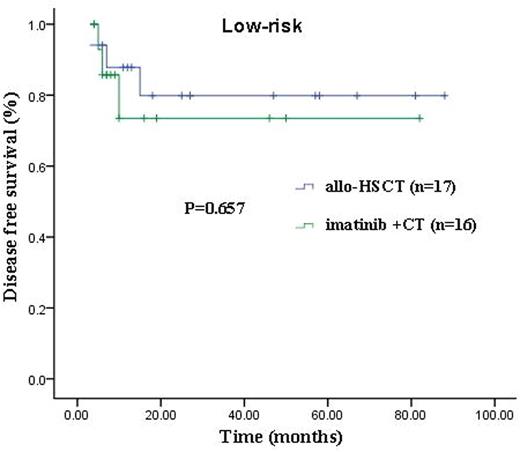
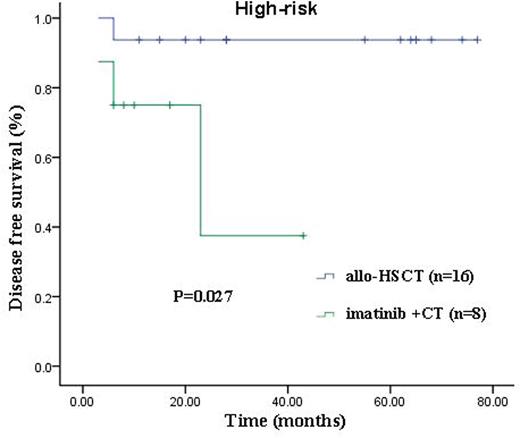
Results: 122 Ph+ALL patients were included. 64 patients were male (52.5%). Median age was 36 years (range, 14-65 years). 2 patients (1.6%) died before response assessment, and 115 (95.8%) achieved CR. With a median followed-up period of 20 months (range, 1-98 months) in all patients and 28 months (range, 4-98 months) in 99 survivors, 65 patients (56.5%) underwent allo-HSCT and 50 (43.5%) received continuous imatinib with chemotherapy. Cumulative incidence of relapse (CIR), disease-free survival (DFS) and overall survival (OS) rates at 3 years were 17.3%, 79.0% and 81.5%, respectively. Multivariate analyses in the total CR patients showed that BCR-ABL reduction <3 logs from baseline after 2 cycles of consolidation chemotherapy (defined as MRD high level; HR=7.7, 95%CI 2.0-25.0, P=0.002; HR=2.9, 95%CI 1.1-7.1, P=0.026; HR=7.6, 95%CI 1.6-13.7, P=0.009) and imatinib plus chemotherapy (HR=7.1, 95%CI 2.6-20.0, P<0.001; HR=6.1, 95%CI 2.4-15.8, P<0.001; HR=5.6, 95%CI 2.0-15.8, P=0.001) were factors associated with increasing CIR and shorter DFS and OS. In addition, WBC equal or more than 30 X 109/L at diagnosis (HR=2.3, 95%CI 1.1-6.2, P=0.032; HR=4.1, 95%CI 1.3-13.2, P=0.016) was associated with shorter DFS and OS. In an attempt to determine whether choice of therapy contributed to outcome differences among patients with or without common poor prognostic factors (WBC equal or more than 30 X 109/L at diagnosis and MRD high level) for DFS and OS, we categorized the entire cohort into low-risk (possessing none of the factors, n=33), intermediate-risk (possessing any one of the factors, n=45), or high-risk (possessing at least 2 factors, n=24). In the low-risk cohort, choice of therapy did not influence the outcomes. In the intermediate- and high- risk cohorts, treatment with allo-HSCT was significantly superior to imatinib plus chemotherapy, with 3-year CIR, DFS and OS rates of 3.4% versus 44.3% (P=0.001) and 6.2% versus 55.6% (P=0.009); 88.2% versus 51.3% (P=0.001) and 93.8% versus 37.5% (P=0.027); 91.7% versus 56.3% (P=0.001) and 93.8% versus 41.0% (P=0.021), respectively. (Figure)
Conclusions Our data suggest that allo-HSCT is a viable option for all patients with Ph+ALL. It is superior to a combination of imatinib and chemotherapy, conferring significant survival advantages to intermediate- and high-risk patients. However, the outcomes of imatinib plus chemotherapy and allo-HSCT are equally good in low-risk patients. For such patients, allo-HSCT may be considered as a salvage potion if there is evidence of TKI(s) resistance so long as the MRD is carefully monitored.
Outcomes between allogeneic stem cell transplantation versus a combination of imatinib and chemotherapy.
Outcomes between allogeneic stem cell transplantation versus a combination of imatinib and chemotherapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.