Abstract
Background: Factor VIII (FVIII) prophylaxis is the standard of care for patients with hemophilia A; however, conventional FVIII products usually require frequent intravenous infusions (3-4 times/week). The safety, efficacy, and prolonged half-life of recombinant FVIII Fc fusion protein (rFVIIIFc) in previously treated children with severe hemophilia A were demonstrated in the phase 3 Kids A-LONG study (NCT01458106, completed) and ASPIRE extension study (NCT01454739, ongoing). Here, we report cumulative long-term data on the safety and efficacy of rFVIIIFc in children <12 years of age in these studies as of the second interim data cut (8 Dec 2014).
Methods: Subjects who completed Kids A-LONG and met the enrollment criteria for ASPIRE could participate in the individualized prophylaxis (IP; 25-80 IU/kg every 2-5 days, or 20-65 IU/kg on Day 1 and 40-65 IU/kg on Day 4 if twice weekly), or the modified prophylaxis (MP; for subjects in whom optimal dosing could not be achieved with IP) treatment groups. Subjects could switch treatment groups in ASPIRE once 12 years of age. For efficacy analyses, data were summarized according to the treatment group in which each subject participated, for the time period they were in that group; thus, subjects may be included in the analysis of more than one treatment group. Outcomes included: incidence of inhibitors (neutralizing antibody value ≥0.6 BU/mL identified and confirmed on 2 separate samples drawn approximately 2 to 4 weeks apart and performed at the central laboratory as measured by the Nijmegen-modified Bethesda assay), adverse events (AEs), annualized bleeding rate (ABR), treatment of acute bleeds, and changes to prophylactic consumption and dosing interval. Outcomes were analyzed over the cumulative duration of Kids A-LONG through the second ASPIRE interim data cut (8 Dec 2014).
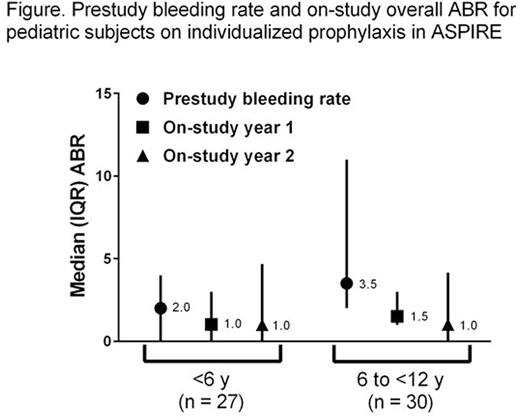
Results: 61/67 subjects who completed Kids A-LONG enrolled in ASPIRE (<6 y, n = 30; 6 to <12 y, n = 31). As of the second interim data cut, 47 subjects were ongoing in ASPIRE; no subjects changed treatment groups during ASPIRE. Median (IQR) cumulative rFVIIIFc exposure days (EDs) for all subjects who received ≥1 intravenous injection (N = 69) were 190.0 (153.0-208.0) days; the median (interquartile range [IQR]) duration of rFVIIIFc treatment was 1.7 (1.5-2.0) years. No inhibitors were reported. The estimated inhibitor incidence rate (95% confidence interval) was 0.0% (0.0, 5.2) overall and 0.0% (0.0, 6.1) in subjects with ≥100 rFVIIIFc EDs (n = 59). The type and incidence of AEs observed were consistent with those expected for a pediatric hemophilia population. 95.7% of subjects reported ≥1 AE on-study; 36/448 were serious and 2/448 were assessed as related to rFVIIIFc treatment by Investigators. 30.4% of subjects experienced ≥1 serious AE; none were assessed by Investigators as related to rFVIIIFc. There were no reports of anaphylaxis or serious hypersensitivity events, and no serious vascular thrombotic events. Median ABRs for subjects on IP (n = 57) were generally lower with rFVIIIFc compared with prestudy FVIII (Figure).In the IP group, the ASPIRE Year 1 and Year 2 median (IQR) spontaneous ABRs were 1.0 (0.0-1.0) and 0.0 (0.0-2.3), respectively, for the <6 y cohort (n = 27), and 0.0 (0.0-1.0) and 0.0 (0.0-0.0), respectively for the 6 to <12 y cohort (n = 30).Overall, 79.8% and 95.8% of bleeding episodes were controlled with 1 or ≤2 intravenous injections, respectively. Among subjects treated with FVIII prophylaxis pre-Kids A-LONG who remained on a prophylaxis regimen (n = 54), the median (IQR) dosing interval was lengthened (prestudy FVIII: 2.3 [2.0, 2.3] days; on-study rFVIIIFc: 3.5 [3.5, 3.5] days) and the median (IQR) total weekly prophylactic consumption was similar (prestudy FVIII: 100.0 [78.0, 120.0] IU/kg; on-study rFVIIIFc: 95.0 [75.0, 113.0] IU/kg).
Conclusions: Longitudinal data from previously treated children with severe hemophilia A treated with rFVIIIFc in Kids A-LONG/ASPIRE confirm long-term safety, with no inhibitors observed in any subjects, and maintained efficacy in the prevention and treatment of bleeding. Low median ABRs were maintained with extended prophylactic dosing intervals, without increased factor consumption.
This research was funded by Biogen and Sobi. Biogen and Sobi reviewed and provided feedback on the abstract. The authors had full editorial control of the abstract and provided their final approval of all content.
Young:Biogen: Consultancy, Speakers Bureau; Kedrion: Consultancy; Novo Nordisk: Consultancy, Speakers Bureau; Baxter: Consultancy. Liesner:Pfizer: Consultancy, Honoraria, Research Funding; Bayer: Consultancy, Honoraria, Speakers Bureau; Octapharma: Consultancy, Honoraria, Research Funding, Speakers Bureau; SOBI: Consultancy, Honoraria, Research Funding, Speakers Bureau; BPL: Consultancy, Honoraria, Research Funding; Baxalta Innovations GmbH, now a part of Shire: Consultancy, Honoraria, Research Funding; Cangene: Research Funding; CSL Behring: Consultancy, Honoraria, Research Funding; Biogen: Consultancy, Honoraria, Research Funding; Grifols: Consultancy, Honoraria. Pasi:Biogen: Consultancy, Honoraria; SOBI: Honoraria, Membership on an entity's Board of Directors or advisory committees; Genzyme: Consultancy, Honoraria; Octapharma: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy, Honoraria. Nolan:Sobi: Research Funding; Biogen: Research Funding. Lethagen:Sobi: Employment. Cristiano:Biogen: Employment, Equity Ownership. Tsao:Biogen: Employment, Equity Ownership. Winding:Sobi: Employment. Mahlangu:Bayer: Research Funding, Speakers Bureau; Biogen: Consultancy, Research Funding, Speakers Bureau; CSL: Consultancy, Research Funding, Speakers Bureau; Novo Nordisk: Consultancy, Research Funding, Speakers Bureau; Roche: Consultancy, Research Funding; Amgen: Speakers Bureau; Biotest: Speakers Bureau; Baxalta: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.