Abstract
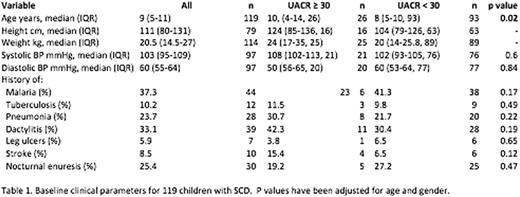
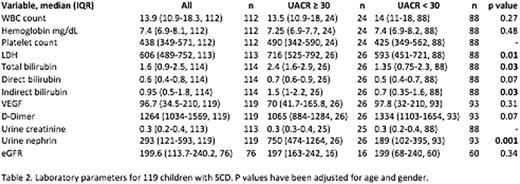
Sickle cell nephropathy (SCN) is a prevalent complication among adults with sickle cell disease (SCD) and has been observed in younger populations, suggesting potential early renal involvement in pediatric patients. Initial hyperfiltration and albuminuria followed by frank proteinuria, leading to declining GFR and eventual end stage renal disease is assumed to be the typical progression of SCN; however, few clinical biomarkers exist to identify early-stage renal disease. We describe the renal profile in 119 children with SCD at Kamuzu Central Hospital in Lilongwe, Malawi and propose a novel urinary biomarker for the identification of children with early renal disease. Among children with confirmed HbSS disease (females 47.9%; median age 9.0 years, IQR: 5, 11), 21.6% were found to have a urinary albumin to creatinine ratio (UACR) 30mg/g or above. Baseline laboratory and clinical parameters stratified by UACR are shown in Tables 1 and 2. Patients with increased levels of UACR were found to be significantly older, and have significantly elevated plasma levels of lactate dehydrogenase (LDH), total bilirubin, and indirect bilirubin when compared to those without albuminuria (p<0.05). No association was seen between albuminuria and either hemoglobin or plasma hemoglobin. Albuminuria was also significantly associated with elevated levels of nephrin, a urinary marker of glomerular injury (p<0.01). Multivariable logistic regression was used to investigate risk factors that are associated with albuminuria (UACR >= 30). Urine nephrin was significantly associated with albuminuria (regression coefficient estimate: 0.00188, SE: 0.000571, p = 0.0010). Additional analysis using a nephrin cut-point of 293 pg/mL, the median value in the cohort, revealed a 17.8 times greater odds of having albuminuria in children with nephrinuria above this value. These data taken together suggests that a significant proportion of children with SCD in Malawi exhibit renal involvement early in life and could be at risk for worsening nephropathy and end-stage renal disease as they grow older. Our data further indicates that urinary nephrin could be utilized as an early marker of glomerular disease in SCN and possibly prompt earlier intervention in these children. The discordant association of albuminuria with clinical markers of hemolysis suggests that hemolysis may not play a substantial role in the pathogenesis of albuminuria in this population. Increased surveillance of children with SCD for renal complications can ultimately inform management strategies to improve outcomes and increase life expectancy among children with SCD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.