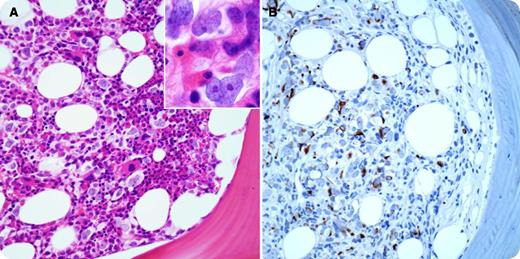
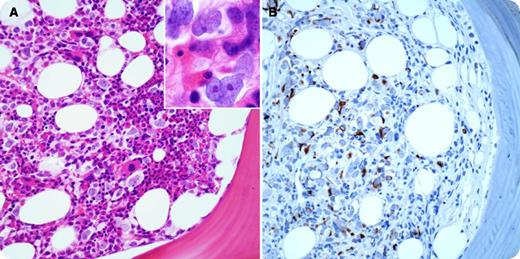
A 64-year-old female with neck/back pain and vaginal bleeding was found to have anemia (hemoglobin 7.4 g/dL), leukocytosis (white blood cell count 22 800/µL), thrombocytosis (platelets 549 000/µL), and elevated creatinine at 2.7 mg/dL and calcium at 17 mg/dL. Image studies demonstrated multiple lytic bone lesions. A plasma cell myeloma was highly suspected. A diagnostic bone marrow (BM) biopsy was promptly performed. BM aspirates showed scattered, large anaplastic cells intimately mixed with hematopoietic cells. The BM core biopsy demonstrated scattered atypical infiltrate in a single-cell fashion in a background of trilineage hematopoiesis (panel A). The infiltrating tumor cells were medium to large in size, having irregular nuclear contours and fine chromatin with small but distinct nucleoli (panel A, inset). Immunohistochemistry was completely negative for pancytokeratin, S-100 protein, and CD45, CD3, CD20, CD30, CD34, CD138, κ, or λ light chain, and essentially ruled out common epithelioid, melanocytic, or hematopoietic neoplasms. However, they were positive for desmin (panel B), myogenin, and myoD1, consistent with metastatic rhabdomyosarcoma in the BM. Further image studies revealed a cervical/uterus mass, which was confirmed as a pleomorphic rhabdomyosarcoma by a subsequent tissue biopsy.
Metastatic rhabdomyosarcoma in the BM presenting as scattered malignant cells as illustrated in the current case is an extremely rare occurrence and poses a great diagnostic challenge, especially when the primary tumor is unrecognized.
A 64-year-old female with neck/back pain and vaginal bleeding was found to have anemia (hemoglobin 7.4 g/dL), leukocytosis (white blood cell count 22 800/µL), thrombocytosis (platelets 549 000/µL), and elevated creatinine at 2.7 mg/dL and calcium at 17 mg/dL. Image studies demonstrated multiple lytic bone lesions. A plasma cell myeloma was highly suspected. A diagnostic bone marrow (BM) biopsy was promptly performed. BM aspirates showed scattered, large anaplastic cells intimately mixed with hematopoietic cells. The BM core biopsy demonstrated scattered atypical infiltrate in a single-cell fashion in a background of trilineage hematopoiesis (panel A). The infiltrating tumor cells were medium to large in size, having irregular nuclear contours and fine chromatin with small but distinct nucleoli (panel A, inset). Immunohistochemistry was completely negative for pancytokeratin, S-100 protein, and CD45, CD3, CD20, CD30, CD34, CD138, κ, or λ light chain, and essentially ruled out common epithelioid, melanocytic, or hematopoietic neoplasms. However, they were positive for desmin (panel B), myogenin, and myoD1, consistent with metastatic rhabdomyosarcoma in the BM. Further image studies revealed a cervical/uterus mass, which was confirmed as a pleomorphic rhabdomyosarcoma by a subsequent tissue biopsy.
Metastatic rhabdomyosarcoma in the BM presenting as scattered malignant cells as illustrated in the current case is an extremely rare occurrence and poses a great diagnostic challenge, especially when the primary tumor is unrecognized.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.