Abstract
Background: The role of combined modality therapy (CMT) in previously untreated patients with primary central nervous system lymphoma (PCNSL) remains unclear. We performed a systematic review of the available evidence regarding the efficacy and long-term neurotoxicity of consolidative radiation therapy in addition to systemic chemotherapy in the upfront management of fit immunocompetent adult patients with PCNSL.
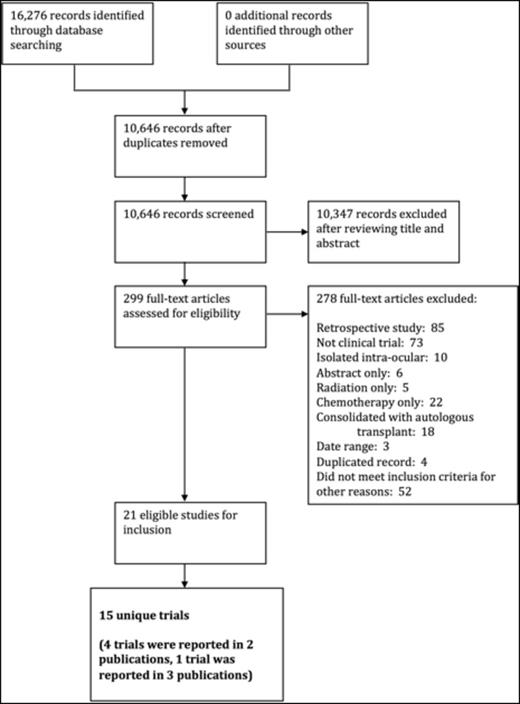
Methods: Peer reviewed literature searches were conducted using the MEDLINE, EMBASE and PubMed databases from 1950 to March 26, 2015. We included all prospective clinical trials (randomized and non-randomized) published on or after January 1, 1998 with at least 20 subjects receiving frontline CMT with CNS-penetrating chemotherapy in addition to radiation therapy. We excluded trials of high-dose chemotherapy followed by autologous stem cell rescue and those involving patients with isolated intra-ocular lymphoma. The primary outcome was overall survival (OS). Secondary outcomes included progression free survival (PFS), overall response rate (ORR), complete remission (CR) rate, partial remission (PR) rate, and incidence of late radiation-induced neurotoxicity. Two reviewers independently performed title and abstract screening, full-text review and data extraction. The Cochrane Risk of Bias Tool was used to assess the quality of randomized trials included in this systematic review.
Results: The literature search yielded 10,646 potentially relevant records for primary screening after de-duplication, of which 299 full-text articles were evaluated. Of the 299 full-text articles reviewed, there were 21 publications eligible for inclusion. These 21 publications represented 15 unique clinical trials (4 trials were reported in 2 publications each, and 1 trial was reported in 3 publications; Figure 1). The included studies involved a total of 1123 enrolled subjects. Of the 15 trials included, there was 1 phase III randomized controlled trial, 1 phase II randomized trial, and 2 non-randomized multi-arm trials. The remaining studies were single arm non-comparator trials. Chemotherapy backbones varied, and planned whole brain radiation therapy (WBRT) doses ranged from 23.4 to 50.4 Gy. Due to variation in follow-up time, it was difficult to compare survival endpoints between studies. In the large multicenter phase III randomized controlled trial comparing 202 patients receiving WBRT to 208 patients without WBRT, there was no difference in OS (32.4 months vs. 36.1 months, p=0.98) however WBRT improved PFS from 9.9 months to 15.4 months (p=0.034) (Korfel et al., Neurology. 2015 Mar 24;84(12):1242-8). Response rates were not consistently reported after completion of both chemotherapy and radiation therapy. Amongst those trials reporting response rates after completion of CMT, the CR rate ranged from 28-87% and the ORR ranged from 56-100%. Although there was variability in the definitions and reporting of delayed-onset neurotoxicity, this complication was common, ranging from 0-45.8%. The Cochrane Risk of Bias Tool was only applicable to the 2 randomized trials in this review. On the basis of clinical heterogeneity, we chose not to statistically pool the results of the included trials together in this systematic review.
Conclusions: We identified a large body of literature assessing the use of CMT in the upfront management of PCNSL. However, only one randomized study addressed the specific role of consolidative radiation therapy with respect to survival, in which there was no benefit to OS. Consolidative WBRT may improve local disease control and PFS, though late neurotoxicity remains a concern. Our review underscores the need for ongoing collaborative efforts between treatment centers to design and conduct large randomized controlled trials.
Buckstein:Celgene: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.