Abstract
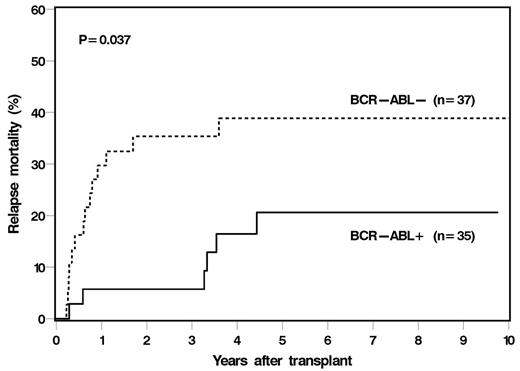
Allogeneic hematopoietic cell transplantation (alloHCT) is a curative therapy for high-risk acute lymphoblastic leukemia (ALL). However, long-term outcomes after alloHCT for adult ALL have not been well described. We conducted a retrospective cohort study of 72 consecutive adult ALL patients who underwent a first myeloablative alloHCT at our institution from January 2000-December 2013. Median age at HCT was 38 yrs (range, 18-62), 40 (56%) were male, 18 (38%) had high HCT CI score, 14 (19%) had prior CNS leukemia and 35 (49%) had BCR-ABL+ disease. Donor source was HLA-matched related donor for 50% patients and 90% received PBSC as graft source. All patients were transplanted in CR (72% were in 1st or 2nd CR) and 92% received T-cell replete grafts. Median time from diagnosis to alloHCT was 5 months (range, 2-90). The incidences of grade II-IV and III-IV acute GvHD, chronic GvHD and extensive chronic GvHD were 43%, 13%, 51% and 36%, respectively. The median follow-up for our cohort is 76 months. At 6 years after HCT, probability of overall survival (OS) was 33% (95% CI, 21-44%) and relapse-free survival (RFS) was 30% (95% CI, 19-42%), and the cumulative incidence of relapse was 36% (95% CI, 25-48%) and non-relapse mortality (NRM) was 37% (95% CI, 26-49%). The most common causes of death were relapse (43%) and infection (21%); majority of relapses occurred within the first 2-years post-transplantation. There were no second cancer related deaths. In multivariable analyses, factors significantly associated with OS were HCT CI score (HR 2.69 for high vs. low/int., P=0.002) and CMV status (HR 2.62 for donor+ vs. others, P=0.05). HCT CI score was the only predictive factor for RFS (HR 2.26 for high, P=0.007). We also compared outcomes by BCR-ABL status. BCR-ABL+ patients were older (median age 42 vs. 36 yrs, p=0.02), had low HCT CI score (34% vs 22%, p=0.01), were more likely to be in CR1 (74% vs. 32%, p=0.002), and as a result, proceeded to HCT sooner after diagnosis (median 4 vs 7 months, p=<0.001). For BCR-ABL+ and BCR-ABL- patients, 6 year OS was 41% and 25%, RFS was 40% and 21%, relapse was 27% and 45% and NRM was 38% and 36% (P=NS for all comparisons). Myeloablative alloHCT can provide long-term survival for selected high-risk adult ALL patients. Relapses are relatively uncommon after 2 years post-transplant. Long-term NRM is high in this population and we did not observe a plateau in its incidence until 7.5 years post-transplant, suggesting the need for long-term follow up to prevent and manage late complications of alloHCT.
Majhail:Gamida Cell Ltd.: Consultancy; Anthem Inc.: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.