Abstract

Background: Childhood and adolescence is characterized by significant physiological alterations including host factors relevant for CML disease course and therapy, e.g. maturation of the immune system and skeletal growth. When compared to adults, minors with CML present with higher disease burden at diagnosis, in particular more frequently in advanced stage of CML, with larger spleen size, and higher leukocyte number. These features are still evident in young adults with CML. Also the genomic breakpoint in the BCR-gene differs when adult and pediatric data are compared. We analyzed pediatric data on clinical and laboratory findings including molecular data from children diagnosed with CML with an emphasis on correlation to age and sex.
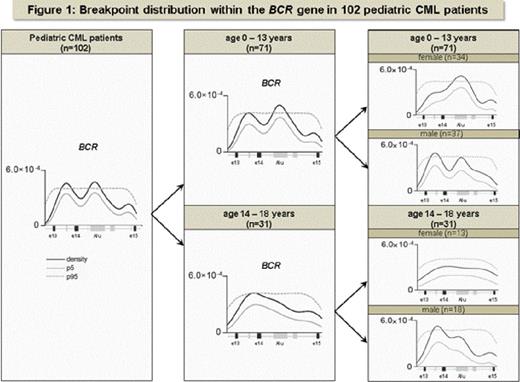
Methods: Data on WBC and spleen size were depicted from the database of 90 German children with CML in CP enrolled into trial CML-PAED II. Taking into account the age-dependent increase of body height during childhood, absolute spleen size below the costal margin was categorized into four categories of relative spleen size: not palpable (I); enlarged moderately (II): age 1-5y <=2cm, age 6-10y <=4cm, age 11-15y <=5cm, age 16-18y <=5cm; enlarged highly (III): age 1-5y >2 - <=7cm, age 6-10y >4 - <=9 cm, age 11-15y >5 - <=13cm, age 16-18 >5 - <=15cm; enlarged excessively (IV): age 1-5y >7cm, age 6-10y >9cm, age 11-15y >13cm, age 16-18 >15cm. DNA was extracted from diagnostic peripheral blood specimen followed by identification of the genomic BCR-ABL breakpoint using long-range PCR. Breakpoint distribution was investigated by Kernel density analysis with respect to age and gender (for details see Krumbholz M et al Genes Chrom Cancer 2012).
Results: WBC (mean 242,000/µl; range 20,000 - 1,150,000/µl) showed a peak at age 10y with a non-significant decline in younger and older children and no significant changes in distribution by gender.
Age-related categorization of spleen size showed that the proportion of patients exhibiting a moderately or highly enlarged spleen, respectively, was more ore less stable in the range of 20 - 25% from age 6 - 15 y while excessively enlarged spleen size was present in one third of 6 - 10y old children and declined with increasing age (see Table 1).
Distribution of spleen size in 90 pediatric patients with CML
| Age [years] No of patients [N] . | 0 - 5 10 . | 6 - 10 27 . | 11 - 15 39 . | 16 - 18 14 . |
|---|---|---|---|---|
| Absolute spleen size and classified relative organ enlargement | N (%) | N (%) | N (%) | N (%) |
| Spleen not palpable | 6 (60) | 5 (19) | 13 (33) | 7 (50) |
| Spleen <= 5 cm b.c.m. Enlarged moderately | 2 (20) 0 ( 0) | 9 (33) 7 (26) | 10 (26) 10 (26) | 3 (21) 7 (50) |
| Spleen >5 - <=15 cm b.c.m. Enlarged highly | 2 (20) 2 (20) | 9 (33) 5 (18) | 10 (26) 8 (20) | 3 (21) 3 (21) |
| Spleen > 15 cm b.c.m. Enlarged excessively | 0 ( 0) 2 (20) | 4 (15) 10 (37) | 6 (15) 8 (20) | 1 ( 8) 1 ( 7) |
| Age [years] No of patients [N] . | 0 - 5 10 . | 6 - 10 27 . | 11 - 15 39 . | 16 - 18 14 . |
|---|---|---|---|---|
| Absolute spleen size and classified relative organ enlargement | N (%) | N (%) | N (%) | N (%) |
| Spleen not palpable | 6 (60) | 5 (19) | 13 (33) | 7 (50) |
| Spleen <= 5 cm b.c.m. Enlarged moderately | 2 (20) 0 ( 0) | 9 (33) 7 (26) | 10 (26) 10 (26) | 3 (21) 7 (50) |
| Spleen >5 - <=15 cm b.c.m. Enlarged highly | 2 (20) 2 (20) | 9 (33) 5 (18) | 10 (26) 8 (20) | 3 (21) 3 (21) |
| Spleen > 15 cm b.c.m. Enlarged excessively | 0 ( 0) 2 (20) | 4 (15) 10 (37) | 6 (15) 8 (20) | 1 ( 8) 1 ( 7) |
b.c.m. : below costal margin
The molecular footprint regarding BCR breakpoint distribution shifted from childhood to adult pattern at the age of 13 years. Also a difference between boys and girls was more pronounced at the prepubertal age (see Fig. 1).
Conclusion: Host factors in growing children are distinct from those of adults. Combined evaluation of adolescent and young adult patients with CML may generate a better understanding of the role of modifying host factors contributing to pathogenesis and development of clinical features of CML. This might form a future basis for age-adapted therapeutic strategies in young individuals with CML.
Suttorp:Novartis, BMS, Pfizer: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract