Abstract
Background:Stenotrophomonas maltophilia (S. maltophilia) bacteremia in allogeneic hematopoietic stem cell transplantation (allo-HSCT) recipients is associated with significant morbidity and mortality rate. Although several predisposing risk factors for S. maltophilia bacteremia following allo-HSCT have been identified, there is no agreement or consistency among clinical factors on whether to predict treatment outcome or not.
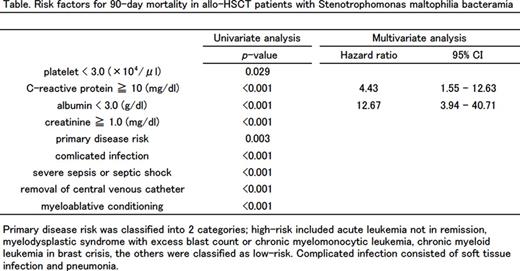
Methods: From January 2005 to December 2014, data on demographic and clinical characteristics, treatment and outcome were collected for all S. maltophilia bacteremia cases observed at an 800-bed tertiary care hospital with a 32-bed transplantation ward. They were analyzed with respect to incidence and 90-day mortality. The risk factors associated with 90-day mortality of allo-HSCT recipients with S. maltophilia bacteremia were also analyzed by Log-rank test according to age, sex, neutropenia, platelet, C-reactive protein (CRP), albumin, creatinine, engraftment, graft-versus-host disease, primary disease risk, severe sepsis or septic shock, complicated infection, and conditioning intensity. Significant variables in the univariate analysis were included in the multivariate Cox proportional-hazards regression model.
Results: A total of 65 patients (47 patients in allo-HSCT recipients and 18 patients in non allo-HSCT recipients) with S. maltophilia bacteremia were identified, with the incidence of 1.17 cases per 100 admissions and 0.35 cases per 1000 patient-days. The incidence was significantly high in allo-HSCT recipients compared to non allo-HSCT recipients (6.53 vs 0.36 per 100 admission, p<0.001) and was apparently increased during the last 2010 to 5 years (1.79 vs 0.63 per 100 admission, p<0.001). The 90-day mortality including all causes of death in allo-HSCT recipients and non allo-HSCT recipients were 43% and 28%, respectively.
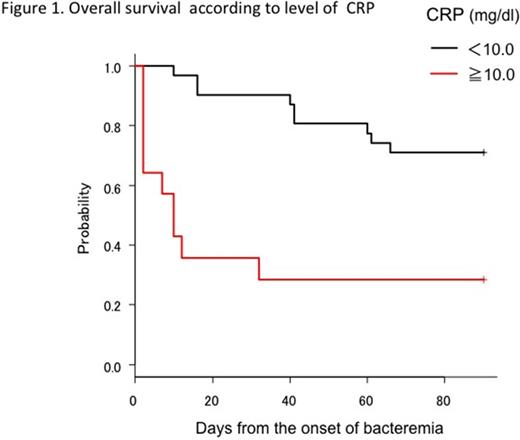
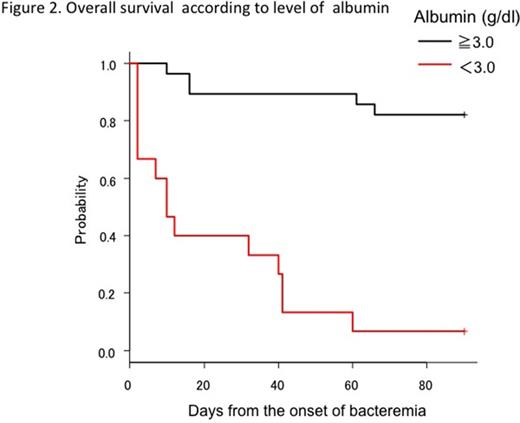
In multivariate analysis, the independent risk factors associated with 90-day mortality of allo-HSCT recipients were a high CRP level (>=10.0 mg/dl) (adjusted hazard ratio [aHR], 4.43; 95% confidence interval [CI], 1.55-12.63; p<0.001) and a low albumin level (<3.0 g/dl) (aHR, 12.67; 95%CI, 3.94-40.71; p<0.001) (Figure 1, 2, and Table). Patients with high CRP or low albumin level were likely to carry the complicated infection or the failure of the initial antimicrobial therapy (p=0.001). Among nine patients with high CRP and low albumin level, five of them had pneumonia at the onset of bacteremia and the others developed pneumonia under effective treatment in median three-days.
Conclusion: The incidence of S. maltophilia bacteremia was increasing during the last 5 years and 90-day mortality was high in allo-HSCT setting compared to non allo-HSCT setting. Higher CRP value or lower albumin level as a result of more complicated infection may predict poor prognosis of patients with S. maltophilia bacteremia.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.