Abstract
Background: At diagnosis, 80% of patients with multiple myeloma (MM) are reported to have osteolytic lesions.MM is characterized by substantial bone destruction, resulting in increased risk of skeletal-related events (SREs), defined as pathological fracture, spinal cord compression, radiation or surgery to bone. SREs are associated with debilitating bone pain, significant morbidity, and increased mortality. SREs also have substantial economic consequences on patients and healthcare systems. Bone-targeting agents (BTAs) approved for the prevention of SREs in MM include intravenous bisphosphonates (IV BPs) zoledronic acid (ZA) and pamidronate (PA). ZA and PA may be used monthly for up to two years and longer for patients who continue to have active or relapsed disease. Given the increased risk of atypical femoral fracture and osteonecrosis of the jaw (ONJ) with cumulative dosing, and medical contraindications (e.g., renal function deterioration), there may be clinician preference to reduce or limit IV BPs. Limited information is available regarding compliance to BTAs in real-world setting in the US. The objective of this study is to examine BTA treatment patterns, including compliance and time to non-persistence among MM patients.
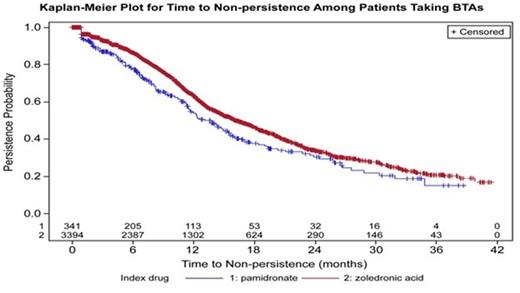
Methods: This retrospective cohort study was conducted using the Oncology Services Comprehensive Oncology Records (OSCER) electronic medical records database, including over 750,000 patients from >200 hematology/oncology practices across the United States. The following selection criteria were used: (1) MM diagnosis (ICD-9CM: 203.0x) between 1st January 2012 and 31st December 2014; (2) ≥18 years of age at MM diagnosis; and (3) initiation of BTA therapy between 1-Jan-2012 and 31-Dec-2014. Patients with solid tumors were excluded. Compliance with BTA therapy was defined as ≥12 administrations in each year of follow-up. Non-persistence was operationalized as either a gap in therapy of ≥90 days or ≥90 days between last administration and last date of follow-up (i.e., discontinuation), or switch from initial BTA. Kaplan-Meier method was used for analysis of time to non-persistence.
Results: Out of 9,617 patients diagnosed with MM, a total of 3,394 (35.3%) patients treated with ZA therapy and 341 (3.6%) treated with PA met inclusion criteria. Majority of the patients were male (ZA: 54.1%, PA: 53.1%), white (ZA: 72.2%, PA: 64.2%), and ≥65 years (ZA: 64.5%, PA: 67.7%). Average time to initiation of therapy from MM diagnosis was 3 months for both ZA and PA. Most of the patients initiated therapy within 3 months (ZA: 76.1%, PA: 75.1%) or 6 months (ZA: 86.3%, PA: 85.6%) of MM diagnosis. Overall the compliance rate was low and declined during follow-up (Table 1). The median time to non-persistence was 16.2 (15.4-17.4) months for ZA and 13.8 (11.5-15.4) months for PA (Fig. 1). Persistence rates declined over the follow-up years, ranging from 86% at 6 months to 34% at 24 months for ZA, and from 77% at 6 months to 30% at 24 months for PA (Fig. 1).
Compliance with BTA therapy over follow-up years
| . | Patients with Minimum 12 Months of Follow-up (N=2,211) . | Patients with Minimum 24 Months of Follow-up (N=899) . | ||
|---|---|---|---|---|
| . | Pamidronate . | Zoledronic Acid . | Pamidronate . | Zoledronic Acid . |
| N | 191 | 2,020 | 95 | 804 |
| Current Users | 191 | 2,020 | 64 | 641 |
| Mean Administrations (Standard Deviation) | 7.6 (4) | 8.3 (3.8) | 7.0 (3.7) | 7.3 (3.9) |
| Switch (n, %) | 28 (14.7) | 39 (1.9) | 3 (3.2) | 9 (1.1) |
| ≥12 Administrations/Year (n, %) | 44 (23) | 553 (27.4) | 10 (15.6) | 127 (19.8) |
| . | Patients with Minimum 12 Months of Follow-up (N=2,211) . | Patients with Minimum 24 Months of Follow-up (N=899) . | ||
|---|---|---|---|---|
| . | Pamidronate . | Zoledronic Acid . | Pamidronate . | Zoledronic Acid . |
| N | 191 | 2,020 | 95 | 804 |
| Current Users | 191 | 2,020 | 64 | 641 |
| Mean Administrations (Standard Deviation) | 7.6 (4) | 8.3 (3.8) | 7.0 (3.7) | 7.3 (3.9) |
| Switch (n, %) | 28 (14.7) | 39 (1.9) | 3 (3.2) | 9 (1.1) |
| ≥12 Administrations/Year (n, %) | 44 (23) | 553 (27.4) | 10 (15.6) | 127 (19.8) |
Conclusions: The treatment landscape in MM has evolved in recent years with clinical trial data supporting improved survival for patients. In this dynamic landscape, it is increasingly important to understand prescribing patterns and patient compliance with BTAs. This analysis indicates there may be limited compliance to BTA therapy in the real-world setting. Potential reasons for non-compliance may include concerns of medical contraindications, patient burden associated with IV administration, or clinician preference. With emerging therapies being evaluated in MM, BTA treatment patterns warrant investigation in future studies.
Qian:Amgen Inc.: Employment. Bhowmik:Amgen Inc.: Employment. Kachru:Amgen Inc.: Employment. Hernandez:Amgen Inc.: Employment. Cheng:Amgen Inc.: Employment. Liede:Amgen Inc.: Employment.
Author notes
Asterisk with author names denotes non-ASH members.