Abstract
Allogeneic HCT improves long-term disease control in pts with ALL, but the treatment-related mortality (TRM) associated with most myeloablative transplant conditioning regimens limits the benefits of HCT. Therefore, we investigated a novel regimen consisting of Clo combined with intravenous (i.v.) Bu in adult pts with ALL undergoing allogeneic HCT. Preliminary results were encouraging1, and we now report on long-term outcomes.
Methods: Clo 40 mg/m2 was infused over 60 min, each dose followed by Bu 130 mg/m2 infused over 3 hours daily for 4 days followed by hematopoietic cell infusion 3 days later. Bu was infused either as a fixed dose per BSA, or to target an average daily AUC of 5,500 microMol-min for pts up to 60 years of age or 4000 microMol-min for pts greater than 60 years, determined by a test dose of Bu at 32 mg/m2 given 48 hours prior to the high dose regimen. Dilantin was administered for seizure prophylaxis. GVHD prophylaxis was based on tacrolimus andmini-MTX, with the addition of rabbit anti-thymocyte globulin (4 mg/kg total dose) for unrelated donor transplants.
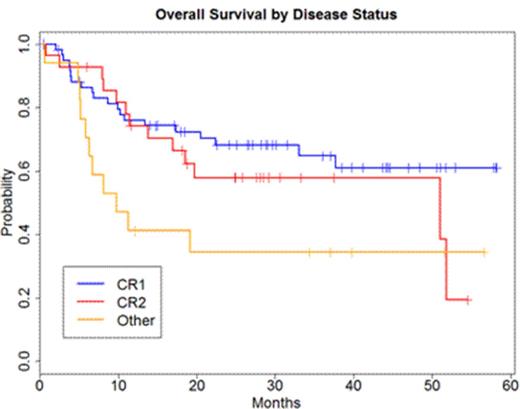
Results: 107 pts (91 B-lineage, 16 T-lineage) with median age 38 years (range 19-64 years) received an allogeneic matched sibling (n=52) or matched unrelated donor (n=55) HCT in CR1 (n=62), CR2 (n=28), or more advanced disease (CR3, n=2; incomplete recovery of counts, n=9; blasts >5%, n=6) .Complete remission was defined by <5% blasts in bone marrow and normal CBC. High-risk cytogenetic profile defined by the presence of t(9;22), t(4;11), or complex cytogenetics was noted in 41% of patients (n=45). The median time from diagnosis to HCT was 9.2 months (range 2.3-118.2 months). The most common grades II-III toxicities were mucositis (93%:70 grade II, 28 grade III) and reversible liver enzyme elevation (84%: 46 grade II, 44 grade III). The incidence of VOD was 6% (5 reversible grade III, 1 grade V); these 6 pts had extensive therapy prior to HCT with median time from diagnosis to HCT of 17.5 months. 104 pts are evaluable for response (early death within 30 days, n=2; recent HCT with less than 30 days follow-up, n=1). Median days to ANC > 0.5 x 109/L and platelet count > 20 x 109/L were 11 (range 10-25 days) and 13 (8-109 days; 8 pts without recovery), respectively. All pts with measurable disease prior to HCT achieved CR by day +30 after HCT. Full donor chimerism by day 30 was achieved in 70% pts; 84% of pts eventually achieved full donor chimerism defined as 100% donor T-cells and myeloid cells. The incidence of grades II-IV and III-IV acute GVHD were 35% and 10%, respectively; 18% pts developed extensive chronic GVHD. With a median follow-up of 2.5 years among surviving patients (0.1-4.9 years), the 2-year overall survival rates for pts transplanted in CR1, CR2, or more advanced disease were 68%, 58%, and 34%, respectively, as illustrated in figure below; 2-year disease-free survival rates were 60%, 40%, and 35%, respectively. Non-relapse mortality (NRM) rates at 100 days and 2 years were 6% and 18%, respectively. Among 9 pts older than 60 years treated with reduced dose Bu in CR1 (n=5), CR2 (n=3) or more advanced disease (n=1), 5 remain alive and disease-free.
Conclusion: The CloBu combination is well-tolerated in this cohort of adult pts with high-risk ALL who received a median of 9.2 months of intensive (mainly HCVAD-based) chemotherapy prior to receiving transplant. Overall survival and NRM compare favorably with traditional TBI-based regimens.
1. Kebriaei et al. Biol Blood Marrow Transplant. 2012 Dec; 18(12): 1819-1826.
Alousi:Therakos, Inc: Research Funding. Andersson:Otsuka Research and Development, Inc.: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.