Abstract
BACKGROUND: Even in the age of kinase inhibitors, the prognosis for patients (pts) with CLL with del(17p) or TP53 mutations remains poor, with the median PFS only 28 mo. for pts with relapsed/refractory del(17p) CLL treated with ibrutinib. High dose methylprednisolone (HDMP) and alemtuzumab (alem) both have activity in 17p disease and work independently of TP53. Prior work has demonstrated that giving HDMP/alem simultaneously is efficacious, but toxic. We hypothesized that giving these agents sequentially with ofatumumab (ofa) would maintain efficacy while decreasing toxicity.
METHODS: This phase II study of ofa/HDMP followed by ofa/alem in CLL pts with 17p deletion or TP53 mutation employed a parallel 2-arm design (treatment-naive (TN) and relapsed/refractory (R/R)). Therapy was the same in both arms and included ofa/HDMP for 2-4 cycles (part A) followed by ofa/alem for 4-24 weeks, up to maximum response (part B). Responders could proceed to alloHSCT or a maintenance phase with ofa given q2 mo and alem given q2 wks (part C). Antimicrobial prophylaxis for PCP, HSV/VZV, and fungal infections was mandatory, as was G-CSF support. The primary objective was to estimate the ORR at the conclusion of the two-part induction therapy in both cohorts. Secondary objectives were to estimate the rate of CR, objective response by compartment, rate of MRD negativity by 4 color flow cytometry, PFS, and OS, rate at which transplant-eligible pts were able to proceed to alloHSCT, and to assess safety. Toxicity was assessed by IW-CLL and CTCAE v4.0. Response assessments by IW-CLL criteria were performed mid-way and at the end of parts A and B, and q6 mo. on part C.
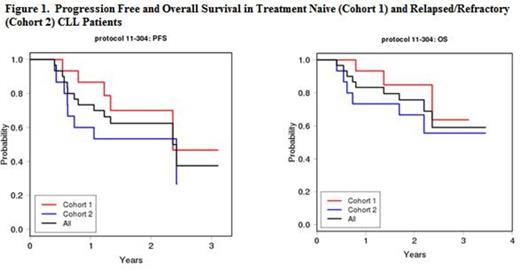
RESULTS: A total of 30 patients were enrolled. Baseline pt characteristics were as follows: TN (n=15): median age 64 (range 45-86), median WBC 58K, Hct 31, Plts 134, B2M 4.3, IGHV unmutated 79%, median %bone marrow (BM) involvement 80%. R/R (n=15): median age 65 (range 58-80), median WBC 31, Hct 33, Plts 114, B2M 4.5, IGHV unmutated 73%, median %BM involvement 60%, median # prior therapies 2 (range 1-4) including 9 pts with prior FCR or FR and 7 pts with prior BR. One patient in each arm had TP53 mutation without 17p deletion, and 4 pts had mut NOTCH1. The median number of copy number changes by SNP array was high, at 12.4 in the TN and 14 in the R/R cohorts. In the TN arm, 14/15 pts moved from part A->B, 5 moved from part B->C, and 5 moved on to alloHSCT in remission. The best ORR for the TN arm was 80% (67% PR, 13% CR), with 12/15 (80%) pts achieving BM MRD negativity. The TN 2-yr PFS and OS are 70% and 85%, respectively. In the R/R arm, 8/15 pts moved from part A->B, 4 moved from part B->C, and 5 moved on to alloHSCT in remission. The best ORR for the R/R arm was 68% (all PRs), with 8/15 (54%) pts achieving BM MRD negativity. The R/R 2-yr PFS and OS are 53% and 67%, respectively. Responses in both arms were independent of TP53 and NOTCH1 mutation status. Studywide, a greater number of somatic mutations was associated with shorter PFS and OS (HR 1.13 per mutation, 95% CI 1.02-1.25, p=0.015 and HR 1.185, 95% CI 1.047-1.341, p=0.0073, respectively).
The most common grade 3/4 toxicities were: neutropenia (33%), thrombocytopenia (20%), anemia (10%). Infectious complications included pneumonia (5 cases, 1 Gr2, 3 Gr3, 1 Gr4), febrile neutropenia (2 cases, both Gr3), and cellulitis (1 case, grade 3). Four pts had low-level CMV reactivation, but no CMV infections occurred. Venous thromboembolism occurred in 3 pts. With a median follow-up time among survivors of 25 mo., 21 of the total 30 pts are still alive, and causes of death included: progressive disease n=6, infection n=3. 12/18 (67%) pts who were transplant eligible were able to proceed to HSCT. Discontinuations were due to: progressive/refractory disease (n=10, including 3 Richter's transformations (R/R n=2, TN n=1)), physician decision (n=2), and unacceptable toxicity (n=1).
CONCLUSION: Ofa/HDMP followed by Ofa/alem is highly active for both TN and R/R CLL pts with del(17p) and/or TP53 mutation. In addition to a robust ORR, we observed a high rate of MRD-negativity in the bone marrow, which allowed most of the transplant-eligible pts to proceed to alloHSCT. Sequential dosing appears to reduce infectious complications compared to concurrent dosing. This regimen is a feasible option for pts with ultra-high risk CLL to facilitate maximal cytoreduction prior to alloHSCT. <>
Davids:Genentech: Other: ad board; Pharmacyclics: Consultancy; Janssen: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.