Abstract
Background
Combination therapy with ATRA and ATO is a standard therapy for relapsed APL. Despite the high complete remission (CR) rate with ATRA-ATO combination therapy, patients administered this combination for relapsed disease may acquire tolerance to ATRA, which reduces the CR rate in relapsed APL patients. Tamibarotene is a novel synthetic retinoid created in Japan with a several-fold-higher differentiation-inducing effect than ATRA, as well as low affinity for cellular retinoic acid-binding protein and absence of binding affinity for RARγ, unlike ATRA. It has been used for treating patients relapsed after ATRA therapy since 2005 in Japan. We conducted a phase III, randomized, open-label, parallel-group, active-controlled, multicenter clinical trial to compare tamibarotene-ATO and ATRA-ATO combination therapies in relapsed APL patients.
Methods
A Phase III, randomized, open-label, parallel-group, active-controlled, multicenter, study of 56 days treatment duration will evaluate the efficacy and safety of 6mg/m2/day Tamibarotene versus 25mg/m2/day ATRA as add-on to 0.15mg/kg/day ATO in subjects with relapsed APL. 71 subjects were randomly assigned to 1 of 2 treatment groups: ATRA-ATO (control group) or tamibarotene-ATO (study group).
Results
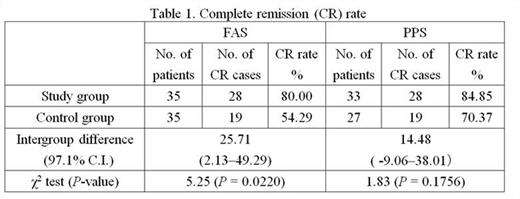
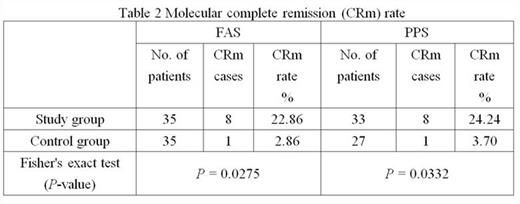
The number of subjects for efficacy analysis constituting a full analysis set (FAS) of all subjects administered study drugs, including drop-outs, was 35 each in the control and study groups. The number of subjects in each per protocol set (PPS), excluding drop-outs, was 27 and 33 in the control and study groups, respectively. CR rate for the FAS was significantly higher in the study group (80.00% vs. 54.29%; P = 0.0220, Table 1). In contrast, CR rate for the PPS was 84.85% and 70.37% for the study and control groups, respectively. The intergroup difference was 14.48% with a 97.1% confidence interval of -9.06 to 38.01%, which fulfilled requirements for non-inferiority of Δ = 0.10. These results verified the non-inferiority of the study to the control group. Of the patients who attained CR, the number who showed complete molecular remission (CRm) was higher in the study group, suggesting that a higher quality of remission was possibly attained in the study group (Table 2).
Serious adverse events occurred in 3 control group patients (intracerebral hemorrhage, 2 and retinoic acid syndrome, 1) and 1 patient in the study group (type I respiratory failure). There was no significant intergroup difference in the incidences of serious adverse events. The most commonly reported adverse reactions included hypertriglyceridemia, hypercholesterolemia, rash, and elevation of ALT and AST levels; there was no significant intergroup difference in the incidences of any of these adverse reactions. Other adverse reaction findings were similar between the groups. Therefore, the tolerability observed in the study group was considered to be similar to that in the control. The only adverse finding that showed an appreciable intergroup difference was leukocytosis, which occurred at a significantly lower frequency in the study group than in the control group. Therefore, the therapeutic regimen of the study group might reduce the risk of retinoic acid syndrome, an important adverse reaction in treatment of APL, when the association of leukocytosis with development of retinoic acid syndrome is considered.
Conclusion
This controlled clinical trial demonstrated the efficacy and safety of combination therapy with tamibarotene and ATO in patients with relapsed APL. Tamibarotene-ATO combination therapy was considered not inferior in efficacy and safety to the standard combination of ATRA and ATO, and may be a useful new combination regimen for treating relapsed APL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.