Abstract
Introduction: Post-Transplant Lymphoproliferative Disorders (PTLD) are a group of heterogeneous disorders that arise as a consequence of iatrogenic immunosuppression for solid organ or allogeneic bone marrow/stem cell transplantation. Though they all arise in a common clinical context, different types of PTLD differ with respect to their underlying biology, clinical presentation and treatment. The aims of this study were to: (1) Define the cell of origin (COO) of monomorphic Diffuse Large B-cell Lymphoma (DLBCL) PTLD and evaluate their impact on clinical presentation and survival and (2) assess the impact of different Rituximab containing treatment regimens on survival outcomes in monomorphic DLBCL PTLD patients.
Methods: We conducted a retrospective review of our institutional databases to identify all the cases of monomorphic PTLD (DLBCL) diagnosed and treated at our medical center from 2000-2013. COO classification into germinal center B-cell like (GCB) and non-germinal center B-cell like (non-GCB) type was performed by immunohistochemistry using the Hans algorithm.
Results: Cell of origin: 40 cases of monomorphic PTLD (DLBCL) were diagnosed during the study interval. Tissue material for COO subtyping was available for 25 patients. By immunohistochemistry 16/25 (64%) were non-GCB and 9/25 (36%) were GCB subtype, median age of presentation being 46 years (range 3-75) and 48 years (range 3-64), respectively. A trend towards EBV positivity (by in situ hybridization for EBV encoded RNA) was noted in the non-GCB group (75% vs. 33%) [p=0.09]. Non-GCB DLBCL PTLD presented earlier post-transplant at a median 1.5 years (range 0.2-15) vs. 3.9 years (range 0.7-17) for GCB cases. When comparing immunosuppressive therapy at the time of PTLD presentation, an association between Tacrolimus therapy and non-GCB phenotype was identified [p=0.03]. Non-GCB DLBCL PTLD demonstrated a trend towards higher rates of extra nodal involvement (88% vs. 44%) [p=0.06] and advanced stage disease (Stage III/IV 75% vs. 33%) [p=0.09]. No significant differences in organ transplanted, LDH, ECOG performance and IPI were observed. While acknowledging the heterogeneity of therapies administered, no significant differences in Progression Free Survival (PFS) (median PFS non-GCB = 17 months vs. GCB = 15 months [p=0.36]) and Overall Survival (OS) (median OS non-GCB = 33 months vs. GCB = 27 months [p=0.22]) were identified.
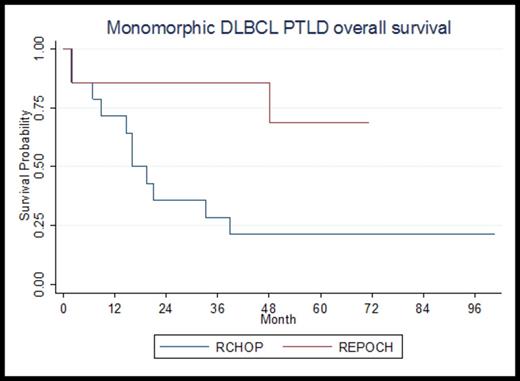
Impact of Treatment: 35 adults (age≥18) were treated at our center. The four most common first line therapies administered were R-CHOP (14), R-EPOCH (7), Palliative Care (5) and Rituximab monotherapy (4). Five patients were given 4 other different therapies. In patients given Rituximab monotherapy, two patients presenting with stage I disease responded while two with stage IV disease progressed. When focusing on patients who commenced R-CHOP or R-EPOCH as their initial therapy, no significant differences in age, stage, LDH, extra nodal disease, ECOG performance status, IPI and immunosuppression therapy was identified between the groups. The complete response (CR) rate for R-CHOP was 50% vs. 71% for R-EPOCH. Primary refractory disease was present in 29% of patients receiving R-CHOP vs. 14% with R-EPOCH. Death during first line therapy occurred equally in both groups (14%). All four primary refractory disease patients in the R-CHOP arm died, while the one patient who was primary refractory to R-EPOCH is alive 3 years post autologous stem cell transplant. R-EPOCH demonstrated prolonged PFS (median PFS R-CHOP = 15 months vs. R-EPOCH not reached [p=0.049]) and prolonged OS (Figure 1) [p=0.036].
Conclusions: (1) In monomorphic PTLD (DLBCL), the non-GCB subtype predominates and is associated with the use of Tacrolimus. It commonly presents with advanced stage disease and extra nodal involvement however, no difference in PFS and OS was noted when compared to GCB DLBCL PTLD. (2) R-EPOCH demonstrated prolonged PFS and OS when compared to R-CHOP. The survival differences reflect the higher rates of primary refractory disease in the R-CHOP group and the inability to salvage patients once they become relapse/refractory. Given the retrospective nature of our analysis, further studies in a larger cohort of patients are ongoing to validate these results.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.