Abstract
Background: We aimed to explore utilization, complication and in-hospital mortality related to Autologous Hematopoietic Stem Cell Transplant (ASCT) in Multiple myeloma (MM) from 1998 to 2011 in United States.
Methods: We used Nationwide Inpatient Sample (NIS) database to isolate multiple myeloma cases undergoing ASCT. Study included adults age >18 years. Patient and hospital demographics were extracted from NIS. Peri-procedural complications were calculated using ICD-9-CM codes. Hierarchical multivariate regression models were formulated to assess predictors of in-hospital mortality and complication.
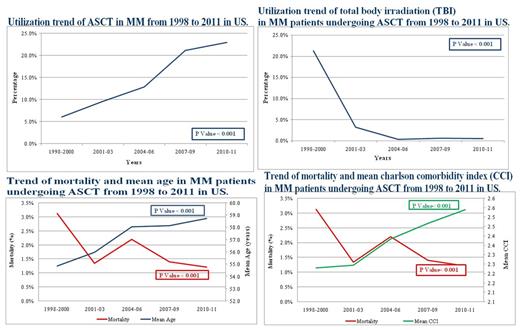
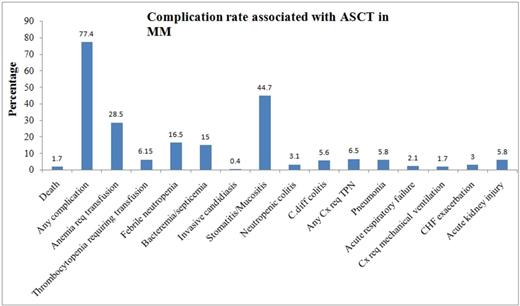
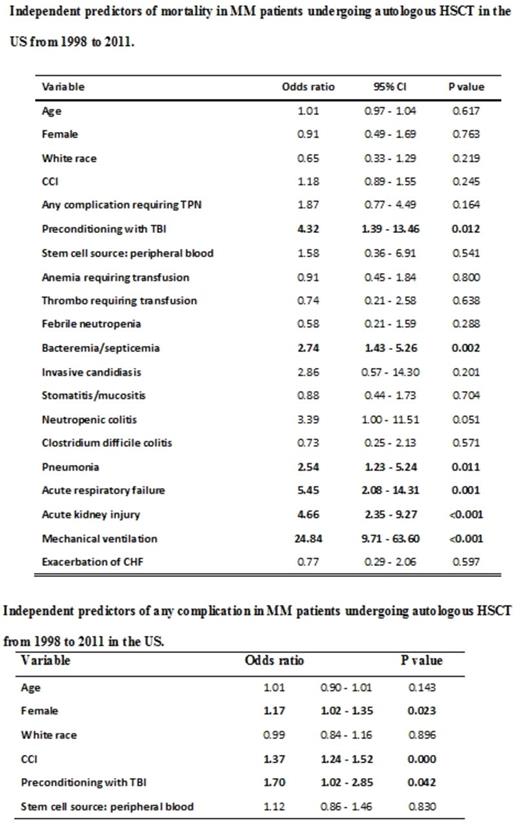
Results: Total of 6,957 (weighted-34,837) were available for analysis. Majority of patients were male (57%), white (57%) who presented to large bed size (78%),teaching (96%) hospital. Utilization of ASCT for MM increased from 5% in 1998 to 21.6% in 2011 (p<0.001). Despite temporal increase in mean age and comorbidites, mortality reduced (2.9 vs. 0.7, p<0.01) significantly from 1998 to 2011. In-hospital complications were common after ASCT with stomatitis (44.7%) being the most common followed by anemia requiring transfusion (28.5%), febrile neutropenia (16.5%) and bacteremia (15.0%). Mechanical ventilation and acute respiratory failure are the strongest predictors of in hospital mortality post ASCT followed by acute kidney injury,total Body irradiation (TBI) and bacteremia. Higher Charlson comorbidity index, female sex and TBI were associated with higher complication rates post ASCT.
Conclusions: Utilization of ASCT for MM patients has increased significantly since 1998 and even though complications are very common in patients undergoing ASCT (77.4%), in-hospital mortality is rare (<2%) and has decreased significantly over the years secondary to decreased use of pre transplant TBI and better transplant care.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.