Abstract
Background: The International Prognostic Index (IPI) is useful for prognostic prediction in patients with diffuse large B-cell lymphoma (DLBCL). Besides the IPI, previous reports demonstrated that some biomarkers (e.g., thymidine kinase [TK] activity and soluble interleukin-2 receptor [sIL-2R] levels) were useful for prognostic prediction in patients with DLBCL. However, few studies have analyzed many biomarkers together. This retrospective study aimed to determine a biomarker that would predict the prognosis of patients with DLBCL most strongly.
Patients and Methods: A total of 781 patients were newly diagnosed with DLBCL at 9 institutions of the Yokohama City University Hematology Group between 2003 and 2012. We analyzed 319 of these 781 patients who were treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) therapy (median 6 cycles) with curative intent, and evaluated 6 biomarkers before R-CHOP treatment. We excluded patients from this study for whom reduction of the initial therapy dose by more than 20% was required owing to any major comorbidities, or who were not evaluated any one of 6 biomarkers, or who were stopped observation during R-CHOP therapy. Using univariate and multivariate analyses, we assessed the association between progression free survival (PFS) and the serum levels of the following 6 biomarkers: lactate dehydrogenase (LDH), sIL-2R, TK activity, beta-2 microglobulin (b2MG), C-reactive protein (CRP), and ferritin. The cut-off values for the 6 biomarkers analyzed were decided by using the receiver operating characteristic curves to determine the association between the values of the biomarkers and PFS. In addition, we assessed the association of the PFS with clinical characteristics including age, sex, presence of B symptoms, presence of bulky masses, Ann Arbor stage, performance status, and presence of extra-nodular lesions. Multivariate analysis includes both 6 biomarkers and clinical characteristics.
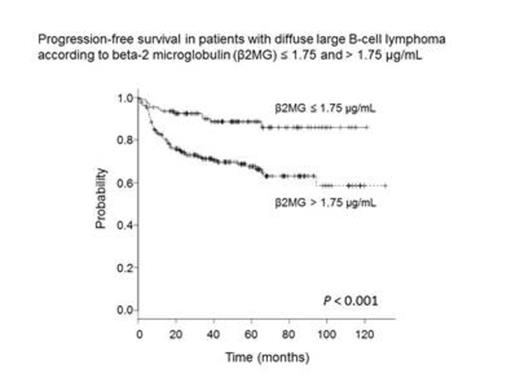
Results: The analyzed patients included 181 men and 138 women, with a median age of 63 years (range, 22–89 years). The median PFS was 40.1 months (range, 0.1–130.8 months). The 3-year PFS rate of the 319 patients analyzed in this study was 77.7% (95% confidence interval [CI], 72.6–82.1%). The cut-off for LDH , sIL-2R, TK activity, b2MG, CRP, and ferritin levels were defined as 1.4 times the upper normal limit, 1660 U/mL, 19 U/L, 1.75 µg/mL, 2.3 µg/mL, and 179 ng/mL, respectively. On univariate analysis, the patients with serum b2MG levels > 1.75 µg/mL showed inferior PFS (n = 210; 3-year PFS rate, 71.2% [95% CI, 64.3–77.0]) compared to those with serum b2MG levels ≤ 1.75 µg/mL (n = 109; 3-year PFS rate, 90.0% [95% CI, 82.1–94.6]). In addition, patients with high levels of LDH, sIL-2R, and CRP as well as high TK activity showed inferior PFS rates compared to patients with low levels of these markers. On multivariate analysis, serum b2MG levels were most strongly correlated with poor PFS (hazard ratio [HR], 2.11; 95% CI, 1.04–4.31; P = 0.04). TK activity as well as CRP, sIL-2R, and ferritin levels did not predict the prognosis of patients with DLBCL.
Conclusion: The serum b2MG level at diagnosis is a useful prognostic marker for patients with DLBCL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.