Abstract
Introduction: While R-CHOP has improved survival for DLBCL, outcome in patients (pts) with relapsed/refractory disease remains dismal and may have worsened since the introduction of immunochemotherapy. High-dose chemotherapy and stem cell transplantation (SCT) offers the best chance of secondary cure, but the majority of patients are ineligible due to age, co-morbidities or disease refractory to salvage chemotherapy. Novel agents will address this unmet medical need; however, their impact is difficult to assess without a reliable historical comparator. Herein, we evaluate the outcome in an unselected population with relapsed/refractory DLBCL following R-CHOP in whom SCT is not feasible.
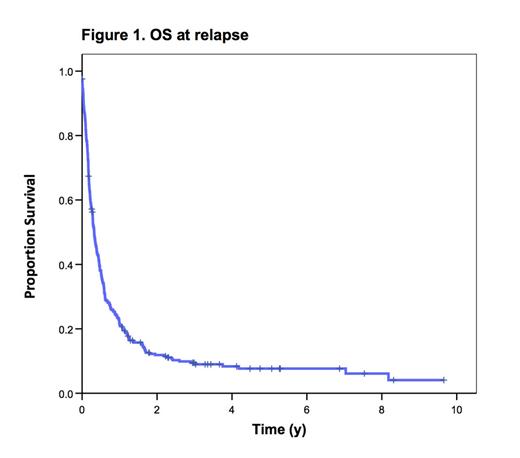
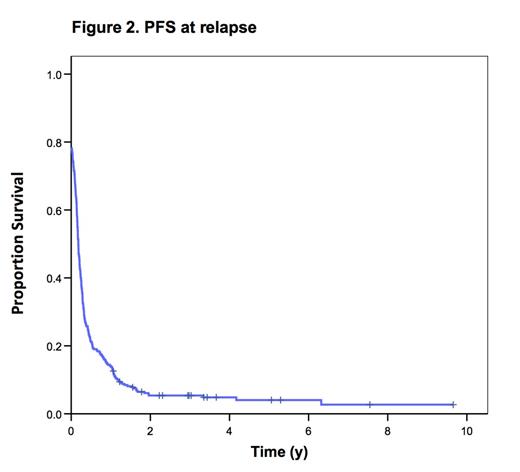
Methods: The BC Cancer Agency Lymphoid Cancer Database was used to identify all pts diagnosed with de novo DLBCL between Dec 2000 to Jan 2013 who were treated with curative intent R-CHOP and subsequently progressed or relapsed. Patients were excluded if they were HIV positive, had CNS involvement at diagnosis, PMBCL, composite/discordant histology or transformed lymphoma. Clinical information at baseline and at relapse/progression was compiled. Overall survival (OS) from relapse was calculated from the date of 1st relapse/progression to death or last follow-up. Progression-free survival (PFS) from relapse was defined as interval from 1st relapse/progression to the date of 2nd relapse, initiation of next line of therapy, death or last follow-up.
Results: 379 pts with relapsed/refractory DLBCL were identified. 53 underwent SCT and were excluded from analysis. The remaining 326 (274 SCT-ineligible and 52 SCT-eligible pts who did not receive SCT due to toxicity or chemo-refractoriness) were analyzed. Response to primary treatment was: 44% CR; 20% PR; 2% SD; 34% PD. 174 (53%) were primary refractory (progression during or within 3 mos of primary R-CHOP). Median time from diagnosis to first recurrence was 7.8 mos (range 0 – 116). Patient characteristics at relapse: median age 70 y (range 21-93); 55% male; 59% elevated LDH; 58% ECOG PS >1; 55% stage III/IV; 18% >1 extra-nodal site; 53% IPI score at relapse > or = 3. 14 (4%) relapsed with an indolent histology only and 74 (23%) exhibited CNS involvement at relapse (54 isolated, 20 concurrent systemic). Treatment at initial relapse: 78 supportive care; 77 radiotherapy (RT) alone; 2 single agent rituximab (for indolent relapse); 168 (R)-chemo +/- RT (79 single agent, 89 multi-agent). (R)-GDP was the most commonly used multi-agent regimen (75%). 1 pt had missing information. Median follow-up for living pts from the time of first relapse was 3 y. Median OS and PFS from relapse for the entire cohort were 3.9 and 2.1 mos, respectively. Outcome was worse for pts with primary refractory disease (median OS 2.5 mos, median PFS 1.7 mos). On multivariate analysis elevated LDH, ECOG PS >1, Stage III/IV and primary refractory status were independent predictors of OS and PFS from relapse. Pts who relapsed > 2 y from diagnosis had a better median OS and PFS from relapse (11 mos and 5.7 mos, respectively). Excluding pts with CNS involvement, pts who received chemo +/- RT (median OS 6.1, median PFS 3.1 mos) or RT alone (median OS 5.7, median PFS 3.3 mos) had a marginally better outcome. Disease control was similar between pts who received multi-agent vs single agent chemotherapy (median PFS 3.3 vs 2.9 mos). Median OS and PFS from relapse for the 74 pts with CNS involvement were 3.3 mos and 2.2 mos, respectively; this was similar compared to the entire cohort. Outcome was also similar between those with isolated CNS recurrence and concurrent systemic disease but 10 pts with isolated CNS relapse survived > 2 yrs. The 14 pts with indolent histology-only relapse had a significantly better outcome (median OS 36 mos, median PFS 12 mos).
Conclusion: The outcome in pts who relapse or progress following R-CHOP is exceedingly poor with standard therapy, with median OS less than 4 mos. Pts who receive treatment at initial relapse fare slightly better, but this may reflect more favorable pt characteristics. Disease control was equivalent for multi-agent vs single agent treatment. While CNS relapse is a rare event in DLBCL, a high proportion of relapsed/refractory pts have CNS disease. The presence of CNS disease did not negatively impact outcome, as outcome was dismal in the entire cohort. Novel treatments are greatly needed and these survival estimates may serve as a comparator to assess their benefit.
Savage:F Hoffmann-La Roche: Research funding to support BCCA Lymphoid Cancer Database Other. Villa:F Hoffmann-La Roche: Other. Shenkier:F Hoffmann-La Roche: Research funding to support BCCA Lymphoid Cancer Database Other. Gerrie:F Hoffmann-La Roche: Other. Klasa:F Hoffmann-La Roche: Other. Connors:F Hoffmann-La Roche: Other. Sehn:F Hoffmann-La Roche: Research funding to support BCCA Lymphoid Cancer Database Other.
Author notes
Asterisk with author names denotes non-ASH members.