Abstract
Kidney is involved in about 70% of patients with AL amyloidosis. End stage renal disease requiring dialysis has deleterious impact on the life of the patients. Recently, Palladini et al proposed that eGFR < 60 ml/min and proteinuria > 5gr/d at diagnosis were able to identify patients with low, intermediate or high probability of progression to dialysis. Also, achievement of at least hemVGPR was associated with favorable renal outcomes. The aim of our study was to validate the above prognostic criteria in a different population and to assess the role of primary therapy with novel agents (bortezomib or lenalidomide) in the renal outcomes of patients with AL amyloidosis. We analyzed 101 consecutive patients with newly diagnosed AL and kidney involvement, which were treated and followed in a single center (Department of Clinical Therapeutics, University of Athens). Because the prognosis of patients with AL is dominated by the degree of cardiac involvement and because many patients die to cardiac complications before reaching dialysis, our analysis was based on competing risk models (proposed by Fine & Gray), in which death without dialysis was treated as competing event.
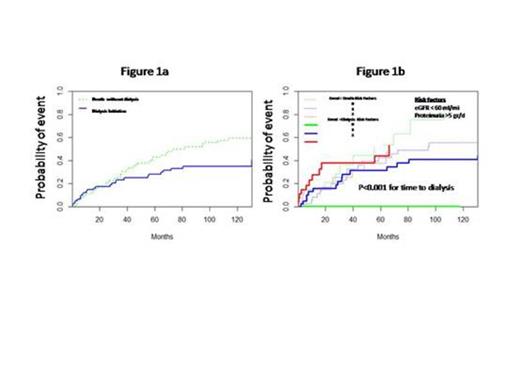
Median age was 65 years (range 40-84), 54% had also cardiac involvement, 27% were Mayo stage 1, 46% stage 2 and 27% stage 3. Median eGFR at the time of diagnosis was 57.5 ml/min; 52% had eGFR <60 ml/min, 29% had eGFR < 30 ml/min and 56% had proteinuria >5 gr/d. Nine (9%) patients who required dialysis at the time of diagnosis were excluded from further analysis. Primary therapy was bortezomib based (mainly VD) in 51%, lenalidomide-based in 29%, MDex in 11%, VAD in 5% and MP in 3%. After a median follow up of 4 years, 28% of the patients required dialysis, 33% died off-dialysis while 40% patients remain alive off-dialysis. One- and 3-year dialysis rates were 14% and 21%, while the incidence of death off-dialysis was 20% and 31% respectively. Thus, even among patients with renal involvement cardiac amyloidosis dominates their prognosis (Figure 1a).
We then evaluated the staging system proposed by Palladini et al. One- and 3-year rate of dialysis for patients with eGFR < 60 ml/min was 20% & 34% vs 9% & 12% for those with eGFR ≥ 60 ml/min (p=0.009); there was no difference in the incidence of death off-dialysis (p=0.345). For patients with proteinuria > 5 gr/d vs those with ≤ 5 gr/d, the respective 1- and 3-year dialysis rate was 23% & 30% vs 5% & 15% (p=0.02) with similar incidence of death off dialysis (p=0.59). Thus, in patients with 0, 1 & 2 risk factors, the 1-year rate of dialysis was 0% vs 13% vs 28% and the 3-year rate was 0% vs 24% vs 37% (p<0.001) (figure 1b). We then evaluated the impact of different types of primary therapy with novel agents (bortezomib or lenalidomide) in renal outcomes. There was no difference in the baseline characteristics of patients who were treated with bortezomib-based vs lenalidomide-based regimens. In univariate analysis bortezomib-based was associated with a longer time to dialysis than lenalidomide-based therapy: 1- and 3- year rate of dialysis was 11.5% vs 26% and 17% vs 37% (p=0.03). There was no difference in the death rates off-dialysis for bortezomib- vs lenalidomide-based therapy (p=0.53). In multivariate analysis, bortezomib-based therapy remained independently associated with a lower probability of progression to dialysis compared to lenalidomide-based therapy (HR: 0.74, 95% CI 0.15-0.95, p=0.039). Hematologic response was associated with renal response as well as longer overall survival. The quality of hematologic response was also associated lower probability of dialysis: 3-year dialysis rate of patients with hemVGPR or hemCR was 10% vs 22% for hemPR vs 28% for patients with no hematologic response to primary therapy (p=0.023). Reduction of proteinuria >20% was associated with excellent renal outcomes: at 3 years no patient who achieved a renal response required dialysis vs. 39% of non renal responders (p<0.001), but death rates off-dialysis were 29% and 36% respectively.
In conclusion, our data confirm previous observations that AL patients with renal involvement who present before severe renal damage occurs (i.e. when eGFR ≥ 60 ml/min and proteinuria ≤ 5gr/d) and which initiate therapy with effective agents, targeting at least hemVGPR, have excellent renal outcomes. In this regard, our data indicate that primary bortezomib-based therapy may be more effective than lenalidomide-based therapy.
Dimopoulos:Celgene: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.