Abstract

DLBCL is the most common lymphoid malignancy, accounting for 30-40% of all Non Hodgkin Lymphomas. Gene expression profiling has identified two main subtypes: Germinal Center B-Cell like (GCB) and Activated B-Cell like (ABC). EZH2 plays an essential role in epigenetic regulation of DLBCL by specifically mono-, bi- and tri-methylating histone H3 lysine 27 (H3K27me1/-me2/-me3). Recurrent somatic heterozygous gain-of-function mutations of EZH2 have been identified in DLBCL, mostly affecting tyrosine 641 (Y641), inducing increased H3K27me3. Novel EZH2 inhibitors are currently being tested in phase 1 and 2 clinical trials in patients with and without EZH2 Y641 mutations, but no study has examined which patients would most benefit from this treatment.
We studied a cohort of 100 patients with DLBCL with available biopsies (96 at diagnosis and 4 at relapse) and developed an immunohistochemical (IHC) assay based on antibodies specifically targeting EZH2, H3K27me3 or H3K27me2. Eighty-six biopsies (12 EZH2 Y641 mutant and 74 WT EZH2) were usable for IHC analysis. Biopsies were scored based on staining intensity and percentage of tumor cells stained, and a me3/me2 score (log of me3 to me2 ratio) was calculated for each patient. Sanger sequencing of EZH2was performed on all patients, GCB/ABC signature was determined by DASL technology based on the expression of 19 genes, and t(14;18) translocation was detected by karyotyping and FISH. The cohort was also extended to 15 patients with EZH2 Y641 mutations and 17 WT EZH2 patients for Next Generation Sequencing (NGS) analysis of a panel of 34 genes involved in lymphomagenesis.
Among our cohort, 45 patients were ABC, 50 were GCB, and 5 were unclassified. Sanger sequencing identified 14 patients with EZH2 Y641 mutations (12 GCB, 1 ABC, 1 unclassified). The t(14;18) translocation was more frequent in patients with EZH2 Y641 mutations (9/14, 64%) (p<10-4). Three distinct IHC profiles emerged based on me3/me2 score: a me3-high/me2-low profile (me3/me2 score>0, n=12/86), a me3-low/me2-high profile (me3/me2 score<0, n=41/86) and an intermediate profile (me3/me2 score=0, n=33/86). Patients with EZH2 Y641 mutations mostly exhibit me3/me2 score>0 profiles (n=7/12), whereas patients with WT EZH2 are split between intermediate (n=29/74) and me3/me2 score<0 profiles (n=40/74) (p<10-5). Survival analysis was performed on patients with biopsies at diagnosis treated with Rituximab. ABC subtype is associated with both inferior OS and PFS within our cohort (p=0.03); among ABC patients, low EZH2 IHC expression is associated with superior OS (p=0.035) and PFS (p=0.02). No correlation was found between prognosis and IHC profile.
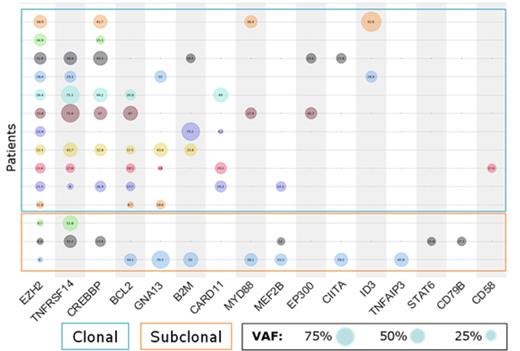
All EZH2 mutations were confirmed by NGS along with their Variable Allele Frequency (VAF). Among GCB EZH2 Y641 mutant patients, a majority of clonal EZH2 mutations (n=11/14) and a minority of subclonal EZH2 mutations (n=3/14) were identified by comparing VAFs of EZH2 and of well-known DLBCL/Follicular Lymphoma driver mutations (including TNFRSF14,CREBBP and MYD88: figure).
Among the 86 patients, a tendency toward a correlation between me3/me2 score and EZH2 VAF exists (p=0.09, r=0.51) and of the 5 patients with EZH2 Y641 mutations presenting a me3/me2 score ≤0, 3 exhibit a VAF inferior to the median. Two also present a subclonal EZH2mutation. These findings could potentially explain their unexpected IHC profile, and possibly decrease their response to EZH2 inhibitor treatment.
Furthermore, 5 WT EZH2 patients present a me3/me2 score>0; 4 are of the ABC subtype, suggesting an EZH2 mutation bypass in ABC patients. NGS analysis also revealed remarkably similar mutational profiles for 2 of these patients, most notably mutations in PRDM1 and PIM1, potentially responsible for EZH2 upregulation by maintaining B cells in GC reaction and possibly justifying EZH2 inhibitor treatment.
EZH2 inhibitors are currently being tested in clinical trials in DLBCL as novel and promising weapons in clinicians’ therapeutic arsenal. This study has shown that IHC and mutational profiles can identify patients most likely to benefit from EZH2 inhibitor treatment by highlighting their in vivo hyper-H3K27me3 status, pinpointing associated activating mutations, and determining EZH2mutation clonality. As such, analyzing these parameters could maximize EZH2 inhibitor benefit and potentially serve to grant access to patients who would otherwise not have been considered.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract