Abstract
Treatment of chronic myeloid leukemia (CML) by tyrosine kinase inhibitors (TKIs, e.g. imatinib, dasatinib) can result in cardiac failure as these drugs exert off-target effects via so far ill-defined mechanisms. Especially in pediatric patients long-term drug exposure is of great concern as this cohort may require life-long treatment for CML. Dasatinib-induced side effects require treatment interruption or dose modification in particular due to hematologic toxicity or cardiac and pleural effusions. Here we investigated the impact of prolonged dasatinib exposure on the growing heart in juvenile rodents. In analogy to clinical data on older adults (La Rosee P, et al, Ann Hematol 2013; in press) we also questioned whether intermittent treatment would result in regression of dasatinib-dependent off-target cardiac toxicity.
Male 4-week old Wistar rats were exposed via the drinking water to dasatinib at a standard-dose (cohort S: 50 µM), at a high-dose (cohort H: 100 µM), and also at the high dose intermittently (cohort I; Mon.-Wed. “on”; Thu.-Sun. “off”), respectively, over 10 weeks continuously. Each cohort comprised 10 animals; controls (cohort K) received water only. Thus, the animals were challenged with drug exposure from shortly after weaning (3 weeks old) over puberty (6-8 weeks old) until young adolescence (14 weeks old). Animals' behaviour, development, and body weight gain was monitored three times weekly. Using a dedicated small animal device echocardiography to determine left ventricular ejection fraction (EF) as well as analysis of blood serums markers indicating cardiac impairment (BNP, IL-6, TNF-alpha, Troponin I) by Luminex assay (Millipore, USA) were performed every two weeks. Necropsy was performed in all rats after spontaneous death while all survivors were sacrificed after 10 weeks of exposure, respectively. Total heart weights and microscopic histopathological changes were examined.
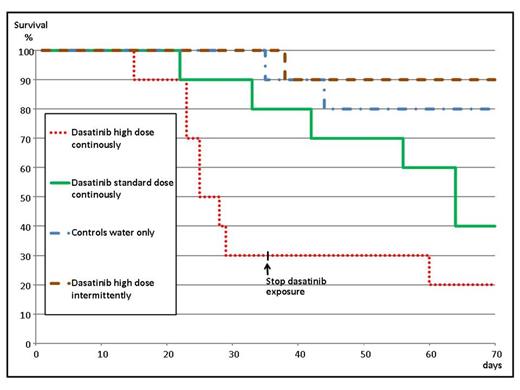
Dose-dependently animals died spontaneously: 8/10 animals from cohort H (high dose continuously), 6/10 animals from cohort S (standard-dose), and 1/10 animals from cohort I (high dose intermittently) , respectively. Two 2/10 controls died from infections. For ethical reason the experiment was terminated in cohort H after 5 weeks of drug exposure. Details on survival time for each cohort are shown in the Kaplan-Meier-Plots below. In concordance with survival data animals also exhibited dose-dependently impaired EF and elevated serum BNP. At necropsy median relative heart weights (% of total body weight) were found increased when compared to controls (0.35 %) for cohort H (0.45 %, p= 0.026), but not significantly higher for cohort S (0.38 %) and cohort I (0.39%), respectively. Findings of heart structural changes comprised a non-significant trend to an increased mast cell (MC) number (median MC counts per visual microscopic field: cohort K= 15 MC; cohort H= 23.5 MC; cohort S= 22.5 MC; cohort I= 17.5 MC).
Continuous long-term exposure to dasatinib at a high dosage is life-threatening to juvenile rats. However, intermittent exposure (treatment and interruption intervals of comparable lengths) will avoid cardiac failure. MCs have been identified to play an important role for cardiac adverse remodelling and increased numbers of MCs have been reported in explanted human hearts with dilated cardiomyopathy and in animal models of experimentally induced hypertension, myocardial infarction, and secondary chronic volume overload (Levick SP, et al, 2011; Cardiovas Res 89:12). Treatment with imatinib has been shown to result in vivo and in vitro in severe bone marrow mast cell depletion via c-kit induced blockade of MC differentiation (Cerny-Reiterer S, et al, 2013; Hematology, EHA abstract P 699). However, it is still unknown whether this also holds true for dasatinib. We conclude that it might be prudent to carefully monitor cardiac function in still growing individuals with CML if treated with dasatinib continuously over long periods.
JT Tauer and N Steinbronn contributed equally to the work.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.