Abstract
Multiple myeloma (MM) and its precursor state monoclonal gammopathy of undetermined significance (MGUS) are two plasma cell dyscrasias whose etiology is largely unknown. Autoimmune disorders (AI) include a variety of conditions, and a history of AI has been found to increase the risk of several malignancies. A personal history of AI is associated with a significantly increased risk of MGUS and to some extent MM. History of AI is a predictor of poor survival in the general population.
The aim of the study was to determine whether a personal history of AI has an impact on survival in MM and MGUS.
Using national Swedish registries we identified 2,719 patients with MM, diagnosed between January 1, 2000, and December 31, 2006, and 4,276 patients with MGUS, diagnosed between January 1, 1988, and December 31, 2006, as well as 28,063 matched control subjects. Through the Swedish Inpatient Registry and Cause of Death Registry, we obtained information on previous AI and on survival, respectively, in patients and controls. We calculated hazard ratios (HR) and 95% confidence intervals (CI). We used the Kaplan-Meier method with log-rank test and Cox proportional hazards model to compare outcome among patients and controls with and without AI. We performed sub-group analyses on seven specific AI conditions; rheumatoid arthritis, pernicious anemia, chronic rheumatic heart disease, ulcerative colitis, polymyalgia rheumatica, giant cell arteritis, and psoriasis. We also performed analyses by M-protein concentration and M-protein isotype (MGUS only).
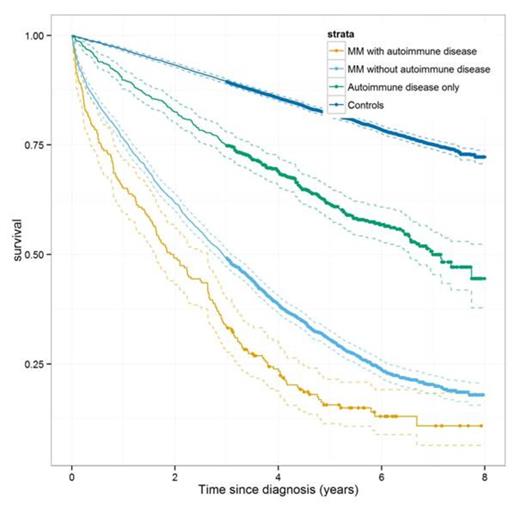
A history of AI was found in 232 MM patients (9%) and in 822 MM controls (8%). Compared to controls with no history of AI, male and female controls with a history of AI had a significantly 2.1-fold increased (95% CI 1.7-2.4, and 95% CI 1.7-2.5, respectively) risk of dying (Figure 1). In patients with MM and a prior history of AI, compared to MM patients with no history of AI, the risk of dying was significantly increased in females (HR=1.5, 95% CI 1.2-2.0) and in males (HR=1.3, 95% CI 1.0-1.7).
Survival in MM patients with and without a personal history of AI, compared to controls with and without a personal history of AI, results for males and females combined.
Survival in MM patients with and without a personal history of AI, compared to controls with and without a personal history of AI, results for males and females combined.
The increased risk of dying after a prior AI was greater in MM patients than in controls for the specific AI conditions rheumatoid arthritis (HR=1.8, 95% CI 1.2-2.5 for controls, HR=1.9, 95% CI 1.3-2.9 for MM patients) and giant cell arteritis (HR=1.9, 95% CI 1.1-3.5 for controls, HR=4.1, 95% CI 1.3-12.7 for MM patients). For the other specific conditions analyzed, the increased risk of dying after a prior AI was smaller in MM patients than in controls.
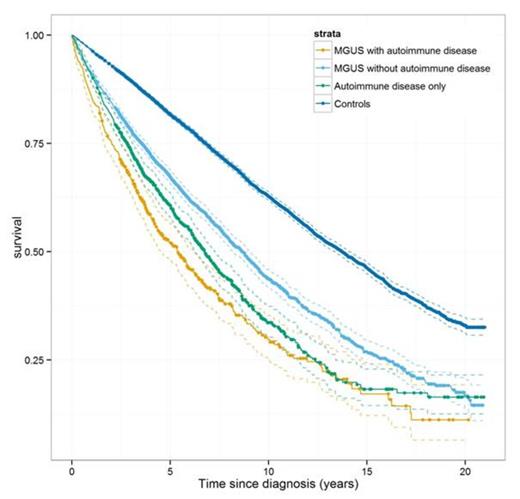
A history of AI was found in 570 MGUS patients (13%) and in 1,312 MGUS controls (8%). Compared to controls with no history of AI, male and female controls with a history of AI had a 1.8-fold (95% CI 1.7-2.1) and a 2.4-fold (95% CI 2.2-2.7) increased risk of dying, respectively (Figure 2). In patients with MGUS and a prior history of AI, compared to MGUS patients with no history of AI, the risk of dying was significantly increased in males (HR=1.3, 95% CI 1.1-1.6) and in females (HR=1.9, 95% CI 1.6-2.3).
Survival in MGUS patients with and without a personal history of AI, compared to controls with and without a personal history of AI, results for males and females combined.
Survival in MGUS patients with and without a personal history of AI, compared to controls with and without a personal history of AI, results for males and females combined.
The increased risk of dying after a prior AI was greater in MGUS patients than in controls for the specific AI condition ulcerative colitis (HR= 1.2, 95% CI 0.6-2.5 for controls, HR=2.6, 95% CI 1.4-5.1 for MGUS patients). For the other specific conditions analyzed, the increased risk of dying after a prior AI was smaller in MGUS patients than in controls.
In patients with MGUS, the effect of a history of AI on survival was not statistically different by isotype (IgA, IgG, or IgM), or by M-protein concentration (above/below 2.0 g/dl) at MGUS diagnosis.
In this large, population-based study aimed at evaluating the influence of a history of AI on survival in MM and in MGUS, we found AI to be a risk factor for survival in both conditions. However, a prior AI was a stronger predictor of survival in individuals without MM or MGUS. For certain AI conditions a history of AI had a greater impact on survival in MM or MGUS patients than in the general population. More attention should be paid to comorbidity as a prognostic factor in MM, and to the need for tailoring therapy according to comorbidity.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.