To the editor:
Marsh et al1 summarize the international experience of stem cell transplantation for X-linked inhibitor of apoptosis protein (XIAP) deficiency. They demonstrate a poor outcome for patients with active hemophagocytic lymphohistiocytosis (HLH) entering transplant (no survivors) and high transplant-related mortality with both myeloablative (7 of 8 patients) and reduced-intensity conditioning (5 of 11 patients). This sensitivity to chemotherapy is predicted by the cellular function of XIAP in regulating apoptosis in hepatocytes.2,3 There is thus a pressing need for transplantation protocols associated with reduced toxicity in this condition. We reasoned that minimal-intensity conditioning using monoclonal antibodies specifically targeting hematopoietic cells might enable engraftment without toxicity to nonhematopoietic tissues. Here we present the first case of a child with XIAP deficiency and treatment-resistant HLH who was successfully transplanted using a monoclonal antibody–based conditioning regimen.4
A 2-year-old child presented with hepatosplenomegaly, pancytopenia, and culture-negative fevers. He progressed to profound HLH associated with multiorgan failure. XIAP deficiency was diagnosed by identifying reduced protein expression and a c.680G>A mutation. He tolerated treatment with the HLH-2004 protocol poorly, developing neurotoxicity (ciclosporin induced posterior reversible encephalopathy), prolonged bone marrow suppression, and infectious complications (Candida and bacterial sepsis, herpes simplex virus stomatitis, parainfluenza II infection).
Immediately prior to transplantation, despite immunosuppression with twice weekly etoposide at 150 mg/m2 and dexamethasone at 0.1 mg/kg/d, his HLH remained refractory (ongoing pyrexias, hepatosplenomegaly, and increased ferritin [6500 µg/L] and triglycerides [2.57 mmol/L]), although his cytopenias responded. He was transplanted from a 10/10 matched unrelated donor using conditioning with alemtuzumab, fludarabine, cyclophosphamide, and anti-CD45 monoclonal antibodies (not currently commercially available; provided from existing stocks by Malcolm Brenner, Baylor College of Medicine). Peripheral blood was the stem cell source (CD34+ 20.5 × 106/kg, CD3+ 4.0 × 108/kg). Graft-versus-host disease prophylaxis consisted of methylprednisolone (1 mg/kg/d), mycophenolate mofitil, and sirolimus. The patient was treated off-study on a clinical governance basis.
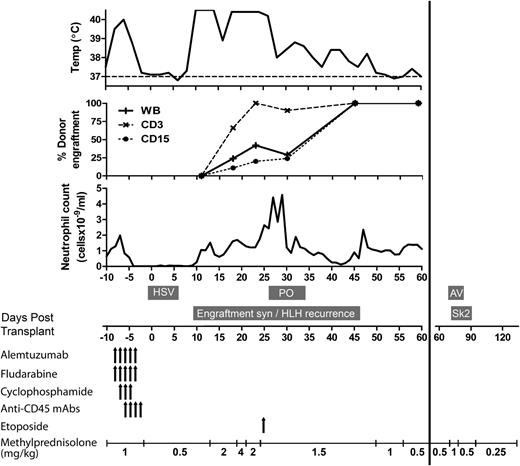
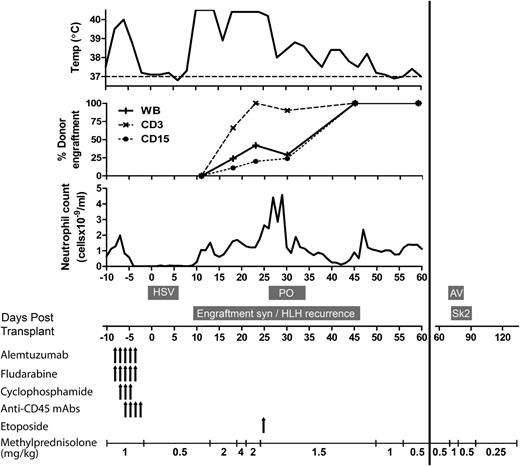
Conditioning was well tolerated with no grade >2 toxicities. His main transplant complication was a syndrome of high fevers (>40.5°C), associated with widespread rash, cardiovascular instability, coagulopathy, and increasing hepatosplenomegaly (Figure 1). These symptoms were contemporaneous with neutrophil recovery, and he was initially treated for presumed engraftment syndrome with 4 mg/kg methylprednisolone. Unfortunately, his symptoms progressed, with development of a capillary leak syndrome associated with pulmonary edema requiring ventilation. His clinical condition and mixed donor chimerism suggested relapsed HLH, and he was treated with a single dose of etoposide. Upon converting to 100% donor chimerism (day 45+ posttransplant) his symptoms and organomegaly resolved. Other complications are summarized in Figure 1. At 400 days posttransplant, he is no longer receiving immunosuppression drugs and has no evidence of HLH. Engraftment studies show 100% donor hematopoiesis in all lineages, with good immune reconstitution.
Clinical course of XIAP-deficient patient with active HLH treated with antibody-based minimal-intensity conditioned stem cell transplant. Time course of conditioning, immunosuppression, neutrophil engraftment, donor chimerism, fevers, and significant complications during the first 140 days following stem cell transplant are shown. Total doses of conditioning drugs were as follows: alemtuzumab, 1 mg/kg; fludarabine, 150 mg/m2; cyclophosphamide, 1 g/m2; anti-CD45 monoclonal antibodies, 1600 µg/kg each of YTH24/54 antibodies; and etoposide, 150 mg/m2. AV, adenoviremia requiring treatment with cidofovir; HSV, herpes simplex virus stomatitis and viremia; mAbs, monoclonal antibodies; PO, pulmonary edema as part of a capillary leak syndrome requiring ventilatory support; Sk2, grade 2 skin graft-versus-host disease treated by increased prednisolone dose; syn, syndrome.
Clinical course of XIAP-deficient patient with active HLH treated with antibody-based minimal-intensity conditioned stem cell transplant. Time course of conditioning, immunosuppression, neutrophil engraftment, donor chimerism, fevers, and significant complications during the first 140 days following stem cell transplant are shown. Total doses of conditioning drugs were as follows: alemtuzumab, 1 mg/kg; fludarabine, 150 mg/m2; cyclophosphamide, 1 g/m2; anti-CD45 monoclonal antibodies, 1600 µg/kg each of YTH24/54 antibodies; and etoposide, 150 mg/m2. AV, adenoviremia requiring treatment with cidofovir; HSV, herpes simplex virus stomatitis and viremia; mAbs, monoclonal antibodies; PO, pulmonary edema as part of a capillary leak syndrome requiring ventilatory support; Sk2, grade 2 skin graft-versus-host disease treated by increased prednisolone dose; syn, syndrome.
Here we demonstrate that, by combining a minimal-intensity immunoablative conditioning regimen with a high stem-cell and T-cell dose graft, XIAP deficiency with uncontrolled HLH can be cured, even in the presence of other independent poor prognostic factors. Although anti-CD45 monoclonal antibodies are not currently commercially available, this case provides proof of principle that antibody-based conditioning can secure curative engraftment with low toxicity for patients with XIAP deficiency and refractory HLH whose prognosis is otherwise extremely poor.1,5
Authorship
Contribution: A.J.J.W., O.N., and R.C. collected, analyzed and interpreted data; K.R., P.V. and P.J.A. designed and performed the study; A.J.J.W. wrote the manuscript; and all authors edited and contributed to the writing of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Austen J. J. Worth, Great Ormond Street Hospital for Children, Molecular Immunology Unit, University College London Institute of Child Health, 30 Guildford St, London, WC1N 1EN United Kingdom; email: a.worth@ucl.ac.uk.