Abstract
Abstract 630
Cancer constitutes a strong risk factor for proximal deep-vein thrombosis (DVT). After a proximal DVT, the risk of being diagnosed a previously undiagnosed cancer in the following years is high. This has justified a cancer screening in this situation, the optimal modalities of which (extensive vs. limited screening) are currently under evaluation. However, little is known on the risk of subsequent cancer in case of symptomatic isolated distal DVT (e.g. infra-popliteal DVT without PE) and symptomatic isolated superficial vein thrombosis (SVT) (e.g. without concomitant DVT and PE). The value of cancer screening is therefore debated in these situations. Yet, each of those two other clinical expressions of venous thromboembolic disease (VTE) in the lower limbs is at least as frequent as proximal DVT.
As compared with patients with a first episode of symptomatic isolated proximal DVT (e.g. without PE), we aim assessing the risk of subsequent cancer in patients with a first isolated distal DVT or with a first isolated SVT. A secondary objective was to assess the influence of anatomical characteristics of distal DVT and SVT (deep calf DVT vs. muscular DVT and SVT on varicose vein vs. SVT on non-varicose vein) on the risk of subsequent cancer.
We analysed the data from the OPTIMEV prospective, observational, multicenter study of consecutive in and outpatients recruited after an objectively confirmed symptomatic VTE and followed up three years. All VTE events were diagnosed via a standardized bilateral whole leg compression ultrasonographic protocol screening the entire deep and superficial venous networks.
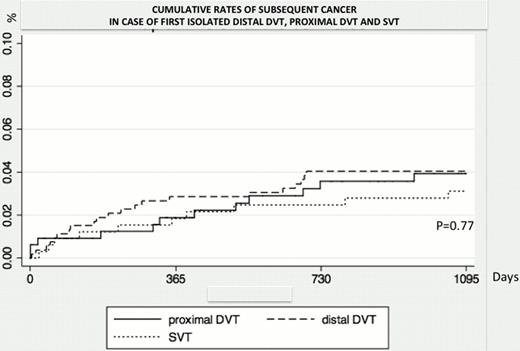
327 patients with a proximal DVT, 536 with a distal DVT, and 329 with an SVT fulfilled our study's inclusion criteria. 2.9% (n=35) of patients were lost to follow-up before 3 years. At 3 years cumulative rates of cancer were similar whatever the kind of VTE considered (Figure 1). Incidence of subsequent cancer was respectively of 3.9% [2.2 – 6.1] in case of proximal DVT, 4.1% (95% CI [2.7 – 6.1]) in case of distal DVT and 3.1% [1.7 – 5.7] in case of isolated SVT.
Neither anatomical characteristics of distal DVT (cumulative rates of subsequent cancer 4.2% [2.3 – 7.4] in case of muscular DVT, 3.7% [1.6 – 8.6] in case of deep calf DVT and 4.3% [1.8 – 9.9] in case of combined muscular and deep calf DVT, p=0.98) nor anatomical characteristics of SVT (cumulative rates of subsequent cancer 1.9% [0.5 – 7.2] in case of SVT on non-varicose vein and 3.4% [1.9 – 7.4] in case of SVT on varicose vein, p=0.4) significantly influenced the risk of subsequent cancer.
This is the largest prospective observational cohort of in and out patients with an objectively confirmed isolated SVT or isolated distal DVT, managed in routine practice, and with a long-term follow-up. Our results only apply to first episodes of isolated SVT or distal DVT. As compared with previous reports on the risk of subsequent cancer in case of VTE, our population of DVT/SVT patients was at low risk of cancer a priori. Indeed, we only included first episodes of VTE, most of which were diagnosed and managed in an outpatient setting and/or were associated with a transient risk factor. Therefore the number of newly diagnosed cancer was limited and we may have lacked statistical power for some sub-group analyses. However our rate of subsequent cancer in proximal DVT patients was in the range of that from recent studies and significantly higher than the expected rate of cancer in the French general population of the same age.
In patients managed in routine practice without previous history of cancer or VTE, every clinical expression of lower limb VTE (proximal DVT, distal DVT and SVT) is associated with a similar risk of subsequent cancer. Anatomical characteristics of distal DVT and SVT do not seem to have a strong impact on this risk. These results suggest that cancer screening should not be modulated according to the deep-proximal, deep-distal or superficial location of lower limb thrombosis.
Cumulative rates of subsequent cancer in case of first symptomatic isolated distal DVT, isolated proximal DVT and isolated SVT in patients without any history of cancer
Cumulative rates of subsequent cancer in case of first symptomatic isolated distal DVT, isolated proximal DVT and isolated SVT in patients without any history of cancer
Cumulative rates of subsequent cancer according to the proximal, distal or superficial location of VTE were estimated with the Kaplan-Meier method and compared with logrank test.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.