Abstract
Abstract 4330
Acute myeloid leukemia (AML) that arises from an antecedent hematologic disorder (most often myelodysplastic syndrome, MDS) or that is related to prior chemotherapy (therapy-related AML, t-AML) carries a poor prognosis. Secondary AML occurs in 16–50% of patients with MDS and in <5% of patients previously treated with alkylating agents or topoisomerase II inhibitors. Although 50–70% of patients with de novo AML achieve complete remission (CR) with conventional induction chemotherapy (i.e., cytarabine plus an antracycline, “7+3”), secondary AML is more resistant to such treatment (40–50% CR rate). This has led to the use in some centers of alternative induction regimens such as FLAG (fludarabine, cytarabine, filgrastim) ± idarubicin (Ida) in patients with secondary AML. FLAG ± Ida has been used in patients with relapsed, high-risk MDS and in relapsed/refractory AML, and has an overall CR rate of 33% when used first-line for secondary AML (Clavio M et al. Leuk Lymphoma 2001 Jan; 40(3–4):305-13). There is currently no published data directly comparing 7+3 to FLAG ± Ida in this setting. The present study was undertaken to compare the effectiveness and safety of FLAG ± Ida and 7+3 induction regimens in patients with secondary AML.
A retrospective medical record review was conducted between January 1, 2007 and September 30, 2011 of all patients with AML aged ≥18 years seen at our institution who had either cytogenetic abnormalities commonly associated with MDS or had received prior alkylating agents or topoisomerase II inhibitors, and received either FLAG ± Ida or 7+3 for initial treatment of secondary AML. Patients with chronic myelogenous leukemia in blast crisis were excluded. The primary outcome was the CR rate after induction chemotherapy. Secondary outcomes were 30-day mortality, hospital and intensive care unit (ICU) length of stay (LOS), sources and types of infections, antibiotic usage, and time to neutrophil recovery. Fisher's exact test was used to compare categorical outcomes (CR, documented infections) between groups. Kaplan-Meier curves and corresponding log-rank tests were used for time-to-event outcomes (hospital stay, ICU days, neutrophil recovery).
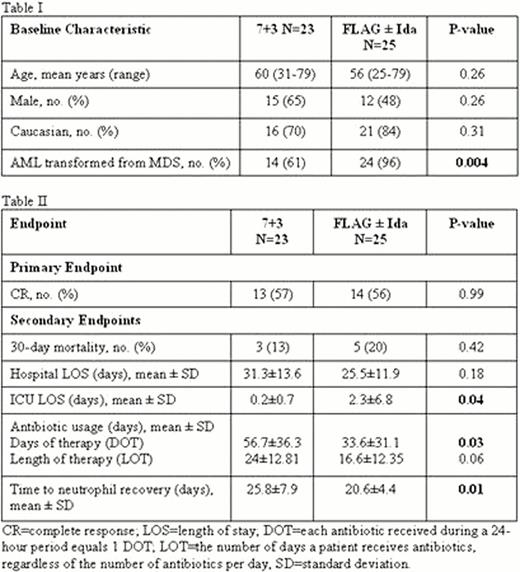
291 charts were reviewed. 48 patients were found to be eligible and were included in the final analysis. There were no significant differences in baseline demographic characteristics between the two treatment groups, with the exception of AML transformation from MDS being more prevalent in the FLAG ± Ida group (Table I). There were no significant differences in CR rates, 30-day mortality, or hospital LOS between the two groups (Table II). 7+3 was associated with a shorter ICU LOS (0.2 ± 0.7 days vs 2.3 ± 6.8 days, p=0.04) but a greater number of days of antibiotic therapy (56.7 ± 36.3 vs 33.6 ± 31.1, p=0.03), while FLAG ± Ida was associated with a shorter time to neutrophil recovery compared with 7+3 (20.6 ± 4.4 days vs 25.8 ± 7.9 days, p=0.01).
In this retrospective study, we found no difference in efficacy between 7+3 and FLAG ± Ida when used as initial induction therapy for patients with secondary AML. Limitations of this study include its retrospective nature, the small sample size and lack of power to detect differences between the groups for both primary and secondary outcomes. A prospectively designed trial is warranted before one regimen can be recommended over the other.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.