Abstract
Abstract 3665
Chemoradiotherapy is considered as one of standard treatment for limited-stage diffuse large B-cell lymphoma (DLBCL). Involved-node radiation therapy (IN-RT) is a newly defined concept for patients with early Hodgkin lymphoma. However, there are as yet few reports of applying the strategy to DLBCL and the optimal radiation treatment fields for patients with limited-stage DLBCL have not been well defined. We conducted a retrospective study to evaluate efficacy and long-term toxicities in limited-stage DLBCL patients receiving IN-RT or involved-field radiation therapy (IF-RT) plus short-course chemotherapy.
Subjects were consecutive patients newly diagnosed as limited-stage DLBCL and receiving local radiation therapy after short-course CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) or R-CHOP (rituximab-CHOP) chemotherapy in our institute from 1993 to 2010. Each patient underwent CT simulation for treatment planning and decided to receive either IN-RT or IF-RT regarding diagnostic imaging after chemotherapy including FDG-PET or PET-CT. The concept of IFRT included the whole initially involved lymph node regions according to the Ann Arbor staging diagram. IN-RT was defined as radiation therapy fields that encompass the initially involved lymph nodes exclusively and to encompass their initial volume with adequate margin less than 3 cm.
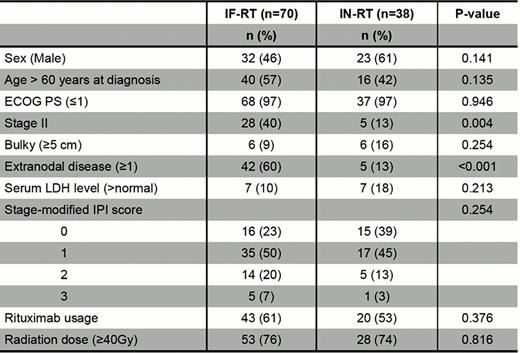
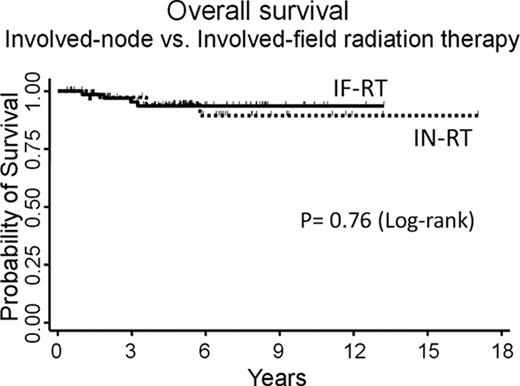
A total of 108 patients were identified, of which 70 patients received IF-RT. The median age was 62 years (range: 19 to 81). Twelve patients (11%) had bulky disease (≥ 5cm). Baseline patients' characteristics were given in Table 1. There was no statistically difference in risk factors as defined by the stage-modified International Prognostic Index score (IPI) between the two groups (P= 0.25). Most patients (94%) received three courses of chemotherapy (range: 2 to 4). Median dose of radiation was 40Gy (range: 23.4 to 51.2). With a median follow-up of 5.5 years (range: 0.35–17), the 5-year overall survival rates were 94% (95%CI: 87 to 97) in all 108 patients, and 94% (95%CI: 79 to 99) and 94% (94%CI: 84 to 98), in the groups of IN-RT and IF-RT, respectively (P=0.76). Estimated 5-year overall survival rates in patients undergoing IF-RT plus CHOP or R-CHOP were 92% and 94%, respectively (P=0.65). Estimated 5-year overall survival rates in patients treated with IN-RT plus CHOP or R-CHOP were 88% and 100%, respectively (P=0.10). Four patients in the IF-RT group experienced relapses [median: 1.8 years after the start of therapy (range: 0.9 to 7.6)], on the other hand, no patient had relapse in the IN-RT group. Three out of the four patients had three adverse risk factors as defined by the stage-modified IPI. Two patients had the relapsed diseases outside radiation fields. Cumulative incidence of relapse at 5 year was 0% and 4.6% (95%CI: 1.2 to 12) in the patients receiving IN-RT and IF-RT, respectively (P= 0.13).
During long-term follow-up, a total of nine patients (8%) developed solid cancer, including skin (n=2), lung (n=2), breast (n=1), gastric (n=2) and bladder (n=2). Seven of which occurred outside radiation fields. No patients developed secondary MDS/AML. Cumulative incidence of secondary malignancy at 5 year was 2.7% (95%CI: 0.20 to 12) and 9.5 % (95%CI: 3.3 to 19) in the groups of IN-RT and IF-RT, respectively, and the cumulative incidence at 10 year was estimated to be 22% (95%CI: 4.0 to 49) and 23% (95%CI: 4.4 to 51) in the groups of IN-RT and IF-RT, respectively. There was no statistically difference in the occurrence of secondary malignancy between the two treatment arms. (P=0.70).
IN-RT with short-course CHOP or R-CHOP chemotherapy could be expected as good as IF-RT in terms of local disease control and could produce excellent survival rates. However, incidence of secondary malignancy in patients receiving IN-RT was not decreased compared to that of IF-RT and the incidence was estimated to have been gradually increased until after 10 years. Physicians might consider the development of follow-up programs for patients with DLBCL undergoing chemoradiotherapy.
Overall survival according to types of irradiation. The 5-year overall survival rates in patients receiving involved-node (IN-RT) and involved-field radiation therapy (IF-RT) were 94% (95%CI: 79 to 99) and 94% (94%CI: 84 to 98), respectively (p=0.76).
Kinoshita:Chugai Pharmaceutical Co., LTD.: Honoraria, Research Funding; Zenyaku Kogyo: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.