Abstract
Abstract  355
355
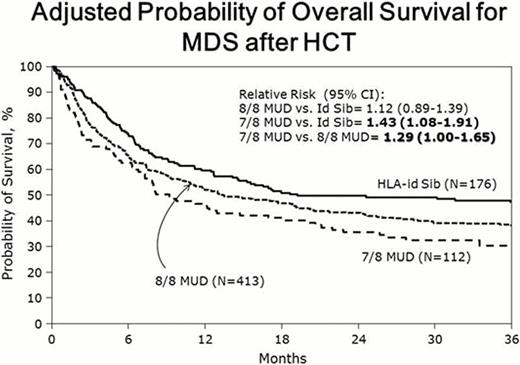
Approximately one-third of patients considered for hematopoietic cell transplantation (HCT) have human leukocyte antigen (HLA) matched related donors (MRD). HLA-matched unrelated donor (MUD) HCT is an alternative approach for the others. A prior CIBMTR analysis showed that transplantation from MUD and MRD donors produces similar survival for patients with acute myelogenous leukemia (AML) (Blood 2012; 119(17):3908–16). Patients with myelodysplastic syndromes (MDS) often are older and have more compromised performance status than patients with AML. There are also differences in disease biology and pre-transplant therapies between the disorders that could lead to different outcomes. Therefore, a disease-specific analysis of post-HCT outcomes after MUD vs. MRD was performed. Outcomes of 701 adult MDS patients who underwent allogeneic HCT between 2002 and 2006 were analyzed (MRD, n=176; 8/8 HLA-A, B, C, DRB1 allele matched MUD, n=413; 7/8 MUD, n=112). Median age was 53 years (range, 22–78). Thirty-one percent had Karnofsky performance scores (KPS) <90% at HCT. Sixty-five percent had advanced disease and 19% had therapy-related MDS. Seventy-seven percent received peripheral blood stem cells; 40% received reduced intensity conditioning regimens. The 100-day cumulative incidence of grades B-D (IBMTR Index) acute graft-versus-host disease (GVHD) was significantly lower in MRD HCT recipients than in 8/8 MUD and 7/8 MUD HCT recipients (42%, 54%, and 57%, respectively; p=0.009). The corresponding 3-year cumulative incidences of chronic GVHD were similar among the three groups (51%, 49%, and 41%; p=0.25). In multivariate analyses, 8/8 MUD HCT recipients had similar DFS and survival rates compared to MRD HCT recipients (relative risk [RR] 1.11 (95% confidence intervals [CI] 0.89–1.39) and 1.24 (95% CI 0.98–1.56), respectively); 7/8 MUD HCT recipients had inferior DFS (RR 1.43, 95% CI 1.08–1.91) and survival (1.62, 95% CI 1.21–2.17) when compared to MRD HCT recipients and when compared to 8/8 MUD HCT recipients (RR 1.29, 95% CI 1.00–1.65 for DFS and 1.30, 95% CI 1.01–1.68 for survival) (Tables 1, 2 and Figure). Differences in outcome were largely related to excess TRM; relapse was not significantly different among the three groups (overall p value=0.33) (Tables 1 and 2). In patients with MDS, transplantation from 8/8 MUD and MRD donors produces similar survival, however, 7/8 MUD HCT is associated with inferior outcomes.
Adjusted 3-Year Cumulative Incidences of TRM, Relapse, and 3-Year Probabilities of DFS and Survival in Adult MDS Patients who Underwent HLA-Identical Sibling (MRD) HCT or 8/8 or 7/8 Matched Unrelated Donor (MUD) HCT from 2002–2006*
| . | MRD Probability (95% CI) . | 8/8 MUD Probability (95% CI) . | 7/8 MUD Probability (95% CI) . | 8/8 MUD vs. MRD P value‡ . | 7/8 MUD vs. MRD P value‡ . | 7/8 MUD vs. 8/8 MUD P value‡ . |
|---|---|---|---|---|---|---|
| TRM | 30 (24-37) | 41 (36-46) | 42 (33-51) | 0.01 | 0.03 | 0.77 |
| Relapse | 32 (25-39) | 24 (20-28) | 27 (19-35) | 0.058 | 0.30 | 0.59 |
| DFS | 40 (33-47) | 35 (30-40) | 29 (21-37) | 0.22 | 0.04 | 0.19 |
| Survival | 47 (40-55) | 38 (34-43) | 31 (22-39) | 0.04 | 0.003 | 0.11 |
| . | MRD Probability (95% CI) . | 8/8 MUD Probability (95% CI) . | 7/8 MUD Probability (95% CI) . | 8/8 MUD vs. MRD P value‡ . | 7/8 MUD vs. MRD P value‡ . | 7/8 MUD vs. 8/8 MUD P value‡ . |
|---|---|---|---|---|---|---|
| TRM | 30 (24-37) | 41 (36-46) | 42 (33-51) | 0.01 | 0.03 | 0.77 |
| Relapse | 32 (25-39) | 24 (20-28) | 27 (19-35) | 0.058 | 0.30 | 0.59 |
| DFS | 40 (33-47) | 35 (30-40) | 29 (21-37) | 0.22 | 0.04 | 0.19 |
| Survival | 47 (40-55) | 38 (34-43) | 31 (22-39) | 0.04 | 0.003 | 0.11 |
Adjusting for patient-related (age, gender, KPS), disease-related (International Prognostic Scoring System stage at diagnosis (d-IPSS), white blood cell count at diagnosis, therapy-related MDS, and disease status at HCT), and HCT-related variables (time between diagnosis and HCT, donor-recipient CMV and gender match, graft type, conditioning and GVHD prophylaxis regimens).
Pointwise pairwise comparison.
Multivariate Analysis for TRM, Relapse, Treatment Failure (Inverse of DFS), and Mortality in Adult MDS Patients who Underwent HLA-Identical Sibling (MRD) HCT or 8/8 or 7/8 Matched Unrelated Donor (MUD) HCT from 2002–2006*
| . | TRM# RR (95 % CI) . | P value . | Relapse± RR (95 % CI) . | P value . | Treatment Failure (Death or Relapse)‡ RR (95 % CI) . | P value . | Mortality∥ RR (95% CI) . | P value . |
|---|---|---|---|---|---|---|---|---|
| 8/8 MUD vs. MRD | 1.37 (1.01-1.85) | 0.03 | 0.78 (0.55-1.10) | 0.16 | 1.11 (0.89-1.39) | 0.33 | 1.24 (0.98-1.56) | 0.06 |
| 7/8 MUD vs. MRD | 1.71 (1.17-2.47) | 0.004 | 0.94 (0.60-1.47) | 0.79 | 1.43 (1.08-1.91) | 0.01 | 1.62 (1.21-2.17) | 0.001 |
| 7/8 MUD vs. 8/8 MUD | 1.24 (0.90-1.70) | 0.17 | 1.20 (0.80-1.79) | 0.37 | 1.29 (1.00-1.65) | 0.04 | 1.30 (1.01-1.68) | 0.03 |
| . | TRM# RR (95 % CI) . | P value . | Relapse± RR (95 % CI) . | P value . | Treatment Failure (Death or Relapse)‡ RR (95 % CI) . | P value . | Mortality∥ RR (95% CI) . | P value . |
|---|---|---|---|---|---|---|---|---|
| 8/8 MUD vs. MRD | 1.37 (1.01-1.85) | 0.03 | 0.78 (0.55-1.10) | 0.16 | 1.11 (0.89-1.39) | 0.33 | 1.24 (0.98-1.56) | 0.06 |
| 7/8 MUD vs. MRD | 1.71 (1.17-2.47) | 0.004 | 0.94 (0.60-1.47) | 0.79 | 1.43 (1.08-1.91) | 0.01 | 1.62 (1.21-2.17) | 0.001 |
| 7/8 MUD vs. 8/8 MUD | 1.24 (0.90-1.70) | 0.17 | 1.20 (0.80-1.79) | 0.37 | 1.29 (1.00-1.65) | 0.04 | 1.30 (1.01-1.68) | 0.03 |
See Table 1 for variables adjusted for in the analysis.
Other Significant factors also include:
KPS and female donor into male recipient.
Disease status at HCT, d-IPSS, and conditioning regimen.
KPS and d-IPSS.
Age, KPS, and d-IPSS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract