Abstract
Abstract 2835
The classical chronic myeloproliferative neoplasms (CMPNs), including essential thrombocytemia (ET), polycythemia vera (PV), and chronic myeloid leukemia (CML), are disorders characterized by accelerated proliferation of hematopoietic tissue. Systemic mastocytosis, also a chronic myeloproliferative neoplasm, has been associated with increased risk of osteoporosis. However, to our knowledge, no data is available on the risk of osteoporosis among patients with classical CMPNs.
We conducted a Danish population-based cohort study of the risk of osteoporosis among patients with ET, PV, and CML using data from the Danish health care system.
ET, PV, and CML patients were identified from Danish National Registry of Patients (DNRP), and linked to the Danish Civil Registration System (CRS) in the study period 1 January 1980 to 31 December 2010. Each Danish resident has a unique, permanent 10-digit civil registry number allowing unambiguous individual-level linkage among all Danish registries. Patients with a first-ever CMPN diagnosis in the DNRP were identified by means of their ICD-8 diagnosis code until 1994 and ICD-10 diagnosis code thereafter. By this means, we established three distinct cohorts of ET, PV, and CML patients. For each CMPN patient, 50 general population comparison cohort members without CMPN were identified in the CRS matched on age, sex, and calendar year, creating three comparison cohorts. Follow-up started 1-year from the date of diagnosis for CMPN patients. The comparison cohort members were assigned the same index date as their index CMPN case.
A diagnosis of proximal femoral fracture was used an indicator of osteoporosis, since this fracture type invariably leads to hospitalization, and therefore would be registered in the DNRP throughout our observation period. The CMPN and comparison cohorts were followed until a diagnosis of femoral fracture, emigration, death, or 31 December 2010, whichever came first. Patients and comparison cohort members with a previous diagnosis of osteoporosis or osteoporotic fractures were excluded.
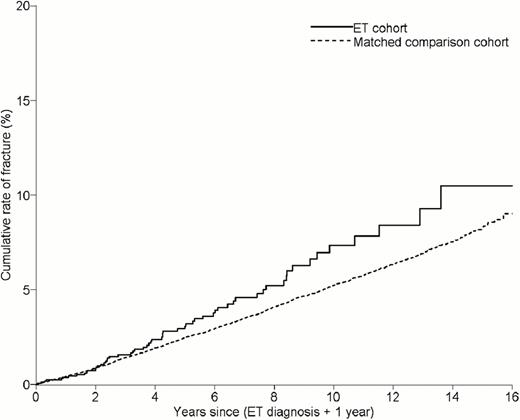
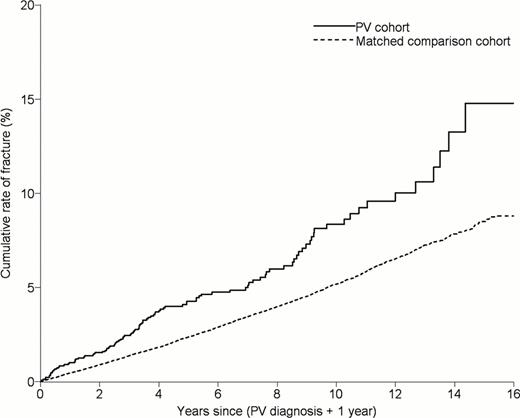
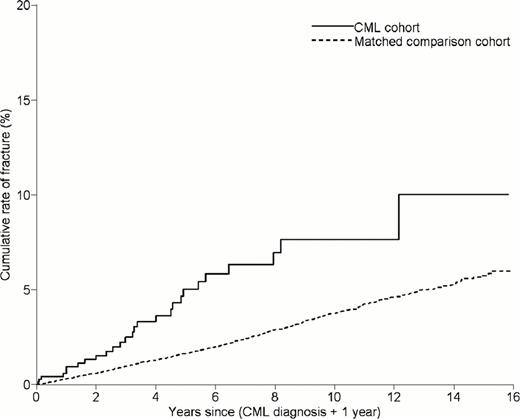
The Kaplan-Meier method was used to estimate the cumulative rate of fractures. Cox regression was used to estimate hazard ratios (HRs) as a measure of relative risk of femoral fracture for each CMPN cohort compared to the comparison cohort, adjusted for comorbidity.
We identified 7,595 MPN patients (1,864 with ET; 4,418 with PV; and 1,313 with CML) and 338,974 comparison cohort members.
The cumulative rate of proximal femoral fractures was higher among CMPN patients than among comparison cohort members, as depicted in the Figures. The rate of fractures per 1,000 person-years were: 6.6 (95% confidence interval (CI): 5.2–8.3) for ET patients [comparison group: 5.3 (95% CI: 5.1–5.4)], 9.9 (95% CI: 8.8–11.0) for PV patients [comparison group: 6.2 (95% CI: 6.1–6.3)]; and 8.2 (95% CI: 6.0–10.7) for CML patients [comparison group: 4.4 (95% CI: 4.3–4.6)].
The resulting adjusted hazard ratios (HR) were: HRET = 1.2 (95% CI: 0.9–1.5), HRPV = 1.8) (95% CI: 1.6–2.0), and HRCML = 2.7 (95% CI: 2.0–3.6).
CMPN patients are at higher risk of osteoporotic fractures than the general population.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.