Abstract
TP53 gene mutations in MDS and AML are, with the exception of cases of isolated del 5q, generally associated with complex karyotype, often including del (17p) (with loss of the remaining TP53 allele) and with poor overall outcome (Fenaux, BJH, 1992; Bejar, NEJM, 2011). They are, in MDS and AML, more specifically generally associated with resistance to chemotherapy, including anthracycline-Ara C combinations and low-dose AraC (Wattel, Blood, 1994), but their correlation with treatment outcome with hypomethylating agents has not been studied. Our aim was to assess the prognostic value of TP53 mutations for response to Azacitidine (AZA) in higher risk MDS, AML with 20–30% blasts or advanced CMML (corresponding to the EU label for AZA).
Patients were treated with AZA (75 mg/m2/d, generally during 7 days every 4 weeks) in 2 centers of the Groupe Francophone des Myélodysplasies. TP53 mutations were detected by the functional FASAY technique, which assesses the transcriptional activity of p53 by co-transfecting an open gap repair plasmid with the product of amplification of TP53 from patients in yeasts whose growth is dependent on the functionality of p53. The detection limit of this technique is around 10–15% (Flaman et al, PNAS 1995). The presence of mutations was subsequently confirmed by direct sequencing using the Sanger method and, more recently, by a Next-Generation Sequencing (NGS) assay using pyrosequencing (GS Junior System, Roche with the IRON II plate design).
72 pts treated with AZA (median n° of cycles of AZA received 4, range 1–7) were analyzed, including 34 MDS according to WHO classification (IPSS high: 9, int2: 13, int1: 6, undetermined: 6), 33 AML with 20–30% blasts and 5 advanced CMML. According to IPSS, karyotype was favorable in 27%, intermediate in 13% and unfavorable in 60% of the pts, including 47% of complex karyotypes.
Response to AZA (according to IWG 2006 criteria) was observed overall in 51% of the pts, including 34% CR, 6% PR, 4% marrow CR, 7% stable disease with HI. Median overall survival (OS) from onset of AZA was 15.6 months, possibly explained by the 47% of complex karyotypes.
29 (40%) patients had a TP53 mutation, detected by FASAY technique and subsequently confirmed by Sanger sequencing or NGS (no false positive with FASAY technique was observed). 22 of the 34 (67%) patients with complex karyotype had a TP53 mutation. In the 7 patients with TP53 mutation without complex karyotype, 3 pts had isolated del(5q), 2 had del (17p) (isolated in 1 pt, with del (20q) in 1 pt), 1 had pentasomy 11 and 1 had +8, del(20q). Ten (77%) of the 13 cases with chromosome 17 rearrangement leading to del (17p) were TP53 mutated.
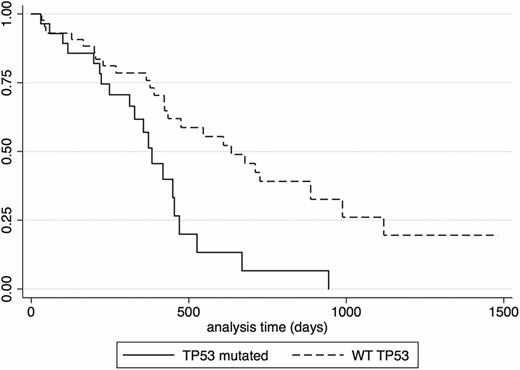
Overall Response to AZA (41% vs 57%, p= 0.227) and CR rate (21% vs 42%, p= 0.073) did not significantly differ between TP53 mutated and wild-type patients. Nevertheless, OS was negatively influenced by the presence of TP53 mutation (median 13 vs 21 months, p= 0.0022, figure 1), complex cytogenetics (median 14 vs 18 months, p=0.0120), WHO AML diagnosis (median 13 vs 21 months for WHO-MDS or CMML, p= 0.0014). By multivariate analysis, marrow blast % (HR 1.03 (1.01–1.05) (p<10-4)) and TP53 mutational status (HR 2.29 (1.06–4.97) p=0.035) were the only 2 factors retaining statistical significance for OS. When the analysis was restricted to WHO MDS and CMML patients, only the presence of TP53 mutation was associated with worse OS in multivariate analysis (HR=4.08 (1.31– 12.7), p=0.015)).
In higher risk MDS (and AML with 20–30% blasts and advanced CMML) patients treated with AZA, the presence of TP53 mutation appears to constitute an independent prognostic parameter of poorer survival.
Overall survival according to TP53 mutational status in patients with MDS treated with Azacitidine.
Overall survival according to TP53 mutational status in patients with MDS treated with Azacitidine.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.