Abstract
Abstract 2024
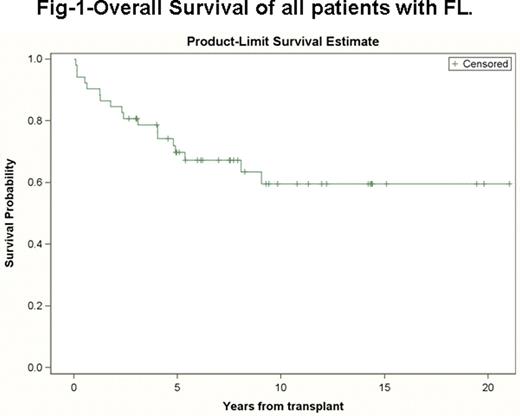
Follicular lymphoma (FL) remains an incurable disease despite the use of immunochemotherapy or autologous stem cell transplant (ASCT). Allogeneic stem cell transplantation (Allo-SCT) remains a viable treatment option in FL because of its associated graft versus lymphoma effect and potential to achieve long term disease control. There is limited data in literature regarding long term outcome of follicular lymphoma post allo-SCT.
Patients and Methods: We identified a total of 52 patients with chemosensitive FL underwent allo-SCT at our centre between 1989 and 2009. 89% were in a chemosensitive remission at time of transplantation. The conditioning regimens included BUCY in 48 (92%) patients. GVHD prophylaxis was cyclosporine and methotrexate until 2009 and subsequently cyclosporine and mycophenolate mofetil. Patients undergoing matched unrelated donor (MUD) transplant received alemtuzumab.
There were 30 (58%) males and 22 (42%) females. The median age at BMT was 45 years (range:24–64) and the median number of prior chemotherapy regimens was 3 (range: 1–6). Fifteen (29%) of patients had only received <3 prior lines of chemotherapy while 36 (69%) had received more than 3 or more lines of therapy at time of transplantation. Prior chemotherapy regimens included anthracyclines in 46 (88%), platinum in 25 (48%), chlorambucil in 25 (46%) and purine analogues in 15 (29%). Twenty three (44%) patients had received prior rituximab and 11 (21%) had received prior radiation therapy (RT). Three (6%) patients had prior ASCT. The median time from diagnosis to transplant was 35 months (range 6–148). All transplants were myeloablative except for one reduced intensity conditioning (RIC) transplant. Forty-five (87%) of patients received matched related donor transplant whereas 2 (4%) received matched unrelated donor (MUD) transplant with the remainder being mismatched donor transplants. The graft source was bone marrow in 35 (67%) and peripheral blood stem cells in 16 (31%). Grade 1–2 acute GVHD was seen in 58% and grade 3–4 in 12%. Chronic GVHD was observed in 50% patients. There was a statistically significant higher incidence of acute GVHD in those who received BM versus PBSC as the graft source although the incidence of cGVHD was not different. Three (6%) patients had relapsed at a median follow up of 68 months. The median time to relapse post-BMT was 54 months (range: 13 – 94). At a median follow up of 68 months (all patients) and 94 months (those who are alive); 34 (65%) patients are alive and well. None relapse mortality was 30%. The overall survival (OS) of entire cohort at 60 months was 70% (Fig-1) and PFS was 68%. Patients, who had achieved chemosensitivity pre transplant, had statistically significant PFS (p=0.04) and OS (p=0.02). In multivariate analysis, number of chemotherapy regimens (</=2) was associated with improved OS (p=0.05).
In summary, myeloablative allo-SCT in younger patients with chemosensitive FL has excellent potential for long-term disease control. With a median follow-up in survivors of 94 months, the NRM remains reasonable. Given inferior results in multiply treated patients, future strategies should identify high risk groups that should be considered for allo-SCT based strategies.
Gupta:Incyte: Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.