Abstract
Abstract 106
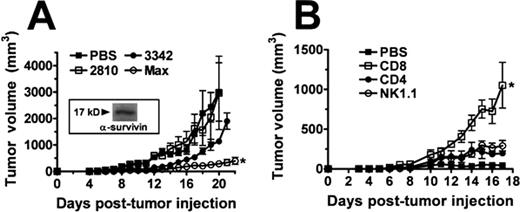
Despite success of the most advanced lymphoma immunotherapy using antibody targeting of the B cell antigen CD20 (Rituximab™), remissions in 50% of treated patients are not durable. The etiology of lymphoma has been extensively studied, though non-viral forms continue to be inadequately understood. Regardless of the initiating events for different forms of lymphoma, a common element shared by these cancers are elevated levels of activated Stat3 (signal transducer and activated of transcription 3) and increased production of Survivin (SVN), a member of the Inhibitor of Apoptosis protein family. SVN and/or Stat3 expression is associated with high-grade lymphoma with poor prognosis and reduced survival. Prior work has shown that knockdown of Stat3 using either pharmacologic or nucleic acid approaches results in steep decreases in SVN production and decreased proliferation of lymphoma cell types with increased apoptosis and cell death. Our focus has been on the H-2b EL4 T-lymphoma cell line, syngeneic to the C57BL/6 mouse. Toward that goal, we have developed a potent Salmonella Typhimurium (ST) based vaccine expressing ST-preferred codon-optimized SVN referred to as Max. This modification is required since SVN antigen is endogenously expressed in ST, and subsequently injected into the cytosol of ST-infected cells by a Type 3 secretion system. The ST vaccine is most efficiently administered by oral gavage, a systemic delivery approach that has superior translational properties than intratumoral administration. When used alone as a therapeutic vaccine, Max can better attenuate growth of established SVN-expressing EL4 tumors (see Figure A) than unmodified native eukaryotic codon forms of SVN (3342) or a Listeria antigen (2810). Increasing the size of the tumor (>50 mm3) before initiation of therapy reduces the efficacy of the SVN vaccine approach. Vaccine efficacy is enhanced leading to complete rejection, if tumor-bearing mice are treated initially by a systemic intravenous route with ST containing a plasmid encoding a short hairpin RNA (shRNA) targeting Stat3 (shStat3). The combined strategy increased tumor cell apoptosis in treated mice providing a mechanism for tumor rejection. We conducted in vitro chromium release assays and discovered that the combined strategy enhanced killing of tumor targets by TIL harvested from ST-treated tumors, while mice with tumors treated with control ST or only one of our ST therapeutics showed insignificant tumor killing. Interestingly, mice treated with shStat3 or Max alone were unsuccessful in rejecting established tumors compared to the combined strategy. We investigated the immunologic mechanism that could account for tumor rejection by conducting in vivo depletion following ST gavage using antibodies specific for CD8 (clone H35), CD4 (clone GK1.5), or NK (clone PK136) subsets by administering 200 μg of depleting mAb every three days after the 1st gavage until sacrifice. In comparison to the small change in tumor growth resulting from depletion of the CD4 or NK1.1 subset, there was a dramatic increase in tumor growth when the CD8 T cell subset was depleted (see Figure B). This difference was statistically significant (*) compared to mock-depleted animals receiving PBS (n=4, 1-way ANOVA, p<0.05).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.