Abstract
Specific internalization of endostatin into endothelial cells has been proved to be important for its biologic functions. However, the mechanism of endostatin internalization still remains elusive. In this study, we report for the first time that both caveolae/lipid rafts and clathrin-coated pits are involved in endostatin internalization. Inhibition of either the caveolae pathway or the clathrin pathway with the use of chemical inhibitors, small interfering RNAs, or dominant-negative mutants alters endostatin internalization in vitro. Intriguingly, cholesterol sequestration by nystatin, a polyene antifungal drug, significantly enhances endostatin uptake by endothelial cells through switching endostatin internalization predominantly to the clathrin-mediated pathway. Nystatin-enhanced internalization of endostatin also increases its inhibitory effects on endothelial cell tube formation and migration. More importantly, combined treatment with nystatin and endostatin selectively enhances endostatin uptake and biodistribution in tumor blood vessels and tumor tissues but not in normal tissues of tumor-bearing mice, ultimately resulting in elevated antiangiogenic and antitumor efficacies of endostatin in vivo. Taken together, our data show a novel mechanism of endostatin internalization and support the potential application of enhancing the uptake and therapeutic efficacy of endostatin via regulating distinct endocytic pathways with cholesterol-sequestering agents.
Introduction
In eukaryotic cells, endocytosis is an important cellular process to internalize various cargo molecules and to regulate signal transduction pathways. Clathrin-coated pits and caveolae are 2 of the most recognizable features of the plasma membrane of mammalian cells. The importance of clathrin-mediated endocytic pathway in uptake, trafficking, recycling, and degradation of the internalized compartments has been extensively studied.1 Caveola/lipid raft–mediated, clathrin-independent endocytosis has emerged as another crucial trafficking pathway.2 Caveolae and lipid rafts, membrane domains enriched in cholesterol and glycosphingolipids, have been found to participate in many cellular events, including cholesterol trafficking and internalization of certain toxins, viruses, GPI-anchored proteins, and many other cargos.3,4
Accumulating evidence supports the notion that the caveola/lipid raft pathway and the clathrin-dependent pathway are not as discrete as traditionally considered. Both caveolae/lipid rafts and clathrin-coated pits have been reported to participate in the endocytosis of many cargoes such as endothelin receptor type A,5 TGF-β receptors,6 B-cell Ag receptor,7 prion,8 bone morphogenetic protein receptor,9 HM1.24,10 and integrins.11-13 Comprehending the mechanisms of distinct endocytic pathways may help discover additional conduits for drug uptake, for instance, the internalization of daidzein-BSA-GdDTPA/CyTE777, a daidzein-BSA–based contrast media, involves 2 competing routes: caveola- and receptor-mediated pathways. Suppression of caveola-mediated internalization by nystatin remarkably increases the uptake of such contrast media by tumor cells.14 Recently, Ishida et al15 reported that a copper chelator enhances the uptake and the therapeutic efficacy of cisplatin in cancerous tissues via attenuating the competing effect of copper on cisplatin uptake.
Endostatin, a 183-aa C-terminal fragment of type XVIII collagen, is a potent inhibitor of angiogenesis.16 It can inhibit the proliferation, migration, and tube formation of endothelial cells, thus eventually impeding angiogenesis and tumor growth.16,17 Specific internalization of endostatin into endothelial cells has been observed and proved to be important, if not essential, for the biofunctions of endostatin.18,19 Although a number of endostatin-binding proteins, such as cell surface nucleolin, integrins, tropomyosin, glypicans, and laminin, have been identified as potential endostatin receptors,19-25 the exact molecular mechanism of endostatin internalization still remains obscure. Endostatin is known to associate with lipid rafts through interaction with integrin α5β1 and caveolin-1 (Cav1).26,27 Cav1 is an adaptor protein and the main coat component of caveola,3 which is abundant in endothelial cells (in which 30% of the cell surface can be occupied by caveolae), adipocytes, smooth muscle cells, and fibroblasts.2 Besides, endostatin-induced lipid raft clustering is observed by Zhang et al28 and Jin et al29 in endostatin-treated endothelial cells and can be disrupted by nystatin or methyl-β-cyclodextrin. In general, these studies indicate the involvement of caveolae/lipid rafts in cell surface attachment of endostatin and the potential role of caveolae/lipid rafts in subsequent internalization of endostatin. However, data on the functions of caveolae/lipid rafts in endostatin internalization are still scarce.
In this study, we aim to study the contributions of caveolae/lipid rafts and other pathways in mediating the internalization of endostatin. By applying pharmacologic and molecular manipulations to selectively disrupt distinct endocytic pathways, we found that internalization of endostatin requires not only caveolae/lipid rafts but also clathrin-coated pits. Remarkably, cholesterol sequestration by nystatin switches endostatin internalization from caveolae/lipid rafts to clathrin-coated pits, leading to a significantly augmented endostatin uptake by endothelial cells. In addition, nystatin-enhanced internalization of endostatin increases its inhibitory effects on endothelial cell migration, tube formation, and VEGF-induced ERK and p38 MAPK activation in vitro. Moreover, combined treatment with nystatin and endostatin selectively enhances endostatin uptake and biodistribution in tumor blood vessels and tumor tissues but not normal tissues, which leads to increased antiangiogenesis and antitumor efficacies of endostatin. Taken together, our results shed light on the mechanism involved in endostatin internalization and indicate the possibility of enhancing the uptake and therapeutic efficacy of endostatin through manipulating distinct endocytic pathways with cholesterol-sequestering agents.
Methods
Reagents, Abs, and plasmids
Nystatin, filipin III, cholesterol, chlorpromazine, FITC-conjugated cholera toxin B subunit (FITC-CTB), and transferrin were from Sigma-Aldrich. Solubilized amphotericin B was from Amresco. Recombinant human endostatin and angiostatin were from Protgen. Biotin-, rhodamine- (Rh-), and FITC-labeling kits (Pierce) were used to label endostatin and transferrin. VEGF 165 was from R&D Systems. Mouse anti–endostatin mAb was from Oncogene Research Products. Abs against Cav1, β-actin, clathrin heavy chain, glypicans-1, phospho-ERK1/2, ERK1/2, phospho-p38 MAPK, and p38 MAPK were from Santa Cruz Biotechnology. Abs against CD31 and angiostatin were from BD PharMingen. Abs against lamin B and transferrin receptor were from Bioworld Technology. Green fluorescent protein (GFP)–tagged Cav1 and clathrin light chain were provided by Du Feng (Tsinghua University). GFP-tagged dominant-negative mutant of Eps15 (Eps15-DIII) and D3Δ2 were provided by Alexandre Benmerah (Cochin Institute).30
Cell culture and transfections
Primary HUVECs were isolated from freshly delivered umbilical cords and maintained as previously described.31 HMEC, an HDMEC cell line (Sciencell) transfected with SV40 large T Ag, was cultured as previously described.32 A549 cell line was purchased from ATCC. Transfection was performed with FuGene HD (Roche Applied Science). Cav1 (5′-CCAGAAGGGACACACAGTT-3′ and 5′-CAGGGCAACATCTACAAGC-3′), clathrin heavy chain (CHC; 5′-GTAATCCAATTCGAAGACC-3′ and 5′-CCUGCGGUCUGGAGUCAAC-3′), and control small interfering RNAs (siRNAs) were from Genechem.
Endostatin internalization assays
HUVECs were treated with culture medium containing indicated concentrations of nystatin, cholesterol, filipin III, or chlorpromazine for indicated time periods, followed by incubation with 5 μg/mL endostatin at 37°C for 30 minutes. Next, cells were washed with acidic buffer (pH = 3.5) and ice-cold PBS to remove cell surface binding endostatin. Subsequently, the cells were examined for endostatin internalization. For VEGF-induced MAPK and ERK activation assay, HUVECs were treated with nystatin or endostatin or both, stimulated with VEGF 165, and then examined for p38 MAPK and ERK phosphorylation.
Isolation of Triton-soluble and -insoluble fractions
Triton-soluble and -insoluble fractions of cell lysate were prepared as previously described.27 In brief, cells were harvested, resuspended in 0.5 mL of 25mM 2-(N-morpholino)ethanesulfonic acid, pH 6.5, 0.15M NaCl that contained 1% Triton X-100 and protease inhibitors (Roche Applied Science), and incubated on ice for 30 minutes. The whole-cell lysates were separated into Triton-soluble and Triton-insoluble fractions with the use of OptiPrep Density Gradient Medium (Sigma-Aldrich).
Flow cytometric analysis
HUVECs were treated with indicated concentration of nystatin, incubated with 20 μg/mL Rh-conjugated endostatin (Rh-endostatin) for 30 minutes at 37°C. Cells in the negative control group were incubated with 20 μg/mL nonconjugated endostatin without nystatin treatment. Afterward, cells were washed with cold acidic buffer to remove unbound and surface-bound endostatin. Cells (105) were then subjected to FACSCalibur flow cytometric system (Becton Dickinson) to monitor the mean fluorescence intensity of Rh-endostatin.
Immunofluorescence
HUVECs (104 cells/mL) were cultured on coverslips and transfected with indicated plasmids for 48 hours. Then the cells were incubated with indicated agents, including nystatin, Rh-endostatin, biotin-endostatin, and FITC-CTB. Cells were further fixed, stained with Abs and 4′,6-diamidino-2-phenylindole (DAPI), and analyzed with a Nikon A1 laser scanning confocal microscope and NIS-Elements Software (Nikon) at room temperature.
Tube formation assay and cell migration assays
Tube formation assay, transwell migration assay, and scratch wound healing assay of HUVECs were performed as described.31 In each assay, HUVECs were treated with saline, nystatin, endostatin, or a combination of nystatin and endostatin. Tube length, migrated cell number, and percentage of wound closure were measured with Image-Pro Plus 5.1 software (Media Cybernetics).
Animal studies
All animal studies were approved by the Institutional Animal Care and Use Committee of Tsinghua University. A549 tumor cells (106) were mixed with Matrigel and injected into the flanks of nude mice subcutaneously. Saline, endostatin (4 mg/kg intravenously), nystatin (4 mg/kg intraperitoneally), or a combination of endostatin and nystatin were injected after the tumor volume approached 0.1 cm3. After 14 daily injections, mice (n = 6/group) were killed, and the tumors were resected, weighed, and applied to immunofluorescent staining. Tumor volumes were measured every 3 days. Rh-conjugated endostatin (20 mg/kg), 125Iodine-conjugated endostatin [specific radioactivity, 1 μCi/μg (0.037 Bq/μg); 0.25 mg/kg], or biotin-conjugated endostatin (20 mg/kg) was intravenously injected into A549 tumor–bearing mice (n = 4/group) combined with or without nystatin (4 mg/kg intraperitoneally) when the tumor volume approached 0.3 cm3. Rh-endostatin uptake by tumor was examined with ex vivo bioluminescence imaging system.33 125Iodine-endostatin uptake levels in selected tissues were counted for radioactivity by a 1470 Wizard Gamma Counter (PerkinElmer). Biotin-endostatin uptake by tumor blood vessels was assessed by immunofluorescent staining with DAPI, tetramethyl-rhodamine isothiocyanate (TRITC)–streptavidin (Pierce), and anti-CD31 staining (FITC).
Results
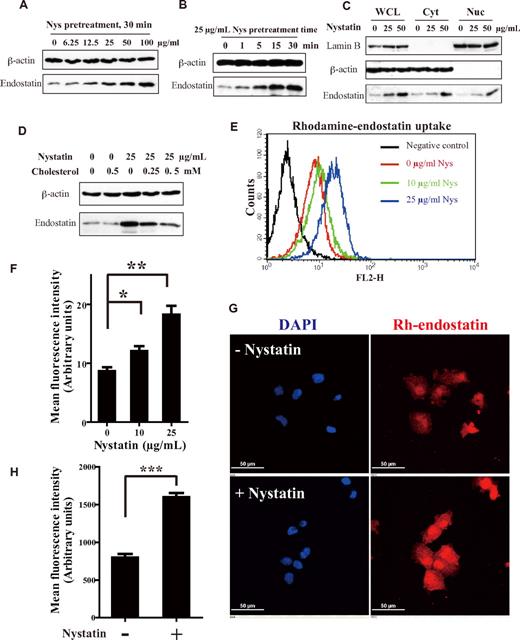
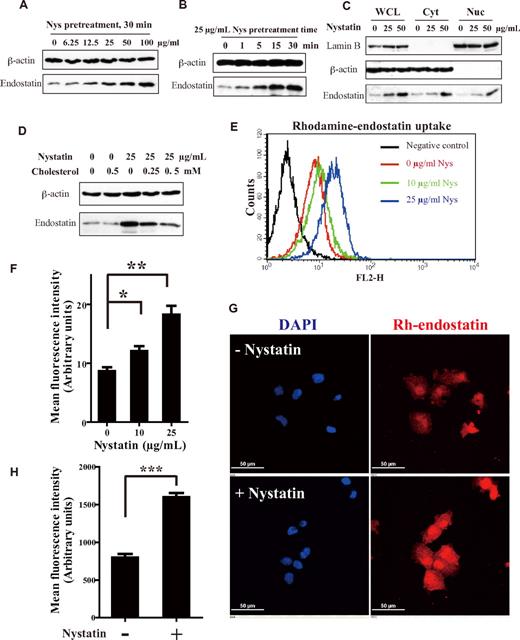
Cholesterol sequestration increases endostatin internalization in endothelial cells
Because endostatin has been found to associate with clustered lipid rafts on plasma membrane, possibly through direct interaction with Cav1, integrin α5β1, and heparan sulfate proteoglycan glypican,26-29 we first queried whether caveolae/lipid rafts are engaged in the process of endostatin internalization. Before endostatin incubation, HUVECs were treated with nystatin, a cholesterol-sequestering, polyene antibiotic agent.34 Nystatin was shown to selectively interrupt caveola/lipid raft-dependent endocytosis without affecting clathrin-mediated internalization.35 Cells were treated with nystatin of various concentrations or for different time courses and then incubated with endostatin. Internalized endostatin was examined by immunoblotting. Unexpectedly, the internalization of endostatin was remarkably increased by nystatin in a dose- and time-dependent manner (Figure 1A-B). The increased endostatin internalization by nystatin was observed not only in the whole-cell lysate but also in the cytosolic fraction and the nuclear fraction (Figure 1C). In addition to nystatin, 2 other commonly used cholesterol-sequestering agents, filipin III and amphotericin B, also exhibited promoting effects on endostatin internalization (supplemental Figure 1A, available on the Blood Web site; see the Supplemental Materials link at the top of the online article). The promoting effect of nystatin on endostatin uptake was also ascertained in human microvascular endothelial cells32 but not in A549 human lung carcinoma cells (supplemental Figure 1B). Consistent with our previous observation,24 internalization of endostatin in cancer cells was negligible, therefore showing no response to nystatin treatment. HUVECs treated with the indicated concentrations of nystatin or other reagents for 24 hours exhibited no substantially diminished cell viability (supplemental Figure 1C). Unlike endostatin, the internalization of angiostatin,36 another angiogenesis inhibitor, remained unaffected on nystatin treatment (supplemental Figure 1D).
Cholesterol sequestration increases endostatin internalization in endothelial cells. (A-B) HUVECs were treated with increasing concentrations (0-100 μg/mL) of nystatin (Nys) for 30 minutes or 25 μg/mL nystatin for increasing time periods (0-30 minutes). Then the cells were incubated with 5 μg/mL endostatin at 37°C for 30 minutes, washed with acidic buffer, and examined for internalized endostatin by immunoblotting. (C) Immunoblot analysis of internalized endostatin levels in whole-cell lysate (WCL), cytosol (Cyt), and nucleus (Nuc). Lamin B and β-actin were used as markers for nuclear and cytoplasm, respectively. (D) HUVECs were resupplied with cholesterol for 30 minutes after nystatin treatment (25 μg/mL, 30 minutes), then applied to endostatin internalization assay. (E) Flow cytometric histogram of Rh-endostatin internalization at 37°C (20 μg/mL, 30 minutes) with 0, 10, or 25 μg/mL nystatin treatment. (F) Mean fluorescence intensity of Rh-endostatin internalization histogram analysis from 3 independent experiments. (G) Immunofluorescence detection of Rh-endostatin in nystatin-treated HUVECs using a Nikon A1 microscope (60×/1.40 NA oil objective). (H) Internalized Rh-endostatin was quantified as the mean fluorescence intensity from ≥ 8 random fields per well of 3 experiments. Scale bar, 10 μm. *P < .05, **P < .01, and ***P < .001. Error bars represent SEMs. P values were calculated with the Student t test.
Cholesterol sequestration increases endostatin internalization in endothelial cells. (A-B) HUVECs were treated with increasing concentrations (0-100 μg/mL) of nystatin (Nys) for 30 minutes or 25 μg/mL nystatin for increasing time periods (0-30 minutes). Then the cells were incubated with 5 μg/mL endostatin at 37°C for 30 minutes, washed with acidic buffer, and examined for internalized endostatin by immunoblotting. (C) Immunoblot analysis of internalized endostatin levels in whole-cell lysate (WCL), cytosol (Cyt), and nucleus (Nuc). Lamin B and β-actin were used as markers for nuclear and cytoplasm, respectively. (D) HUVECs were resupplied with cholesterol for 30 minutes after nystatin treatment (25 μg/mL, 30 minutes), then applied to endostatin internalization assay. (E) Flow cytometric histogram of Rh-endostatin internalization at 37°C (20 μg/mL, 30 minutes) with 0, 10, or 25 μg/mL nystatin treatment. (F) Mean fluorescence intensity of Rh-endostatin internalization histogram analysis from 3 independent experiments. (G) Immunofluorescence detection of Rh-endostatin in nystatin-treated HUVECs using a Nikon A1 microscope (60×/1.40 NA oil objective). (H) Internalized Rh-endostatin was quantified as the mean fluorescence intensity from ≥ 8 random fields per well of 3 experiments. Scale bar, 10 μm. *P < .05, **P < .01, and ***P < .001. Error bars represent SEMs. P values were calculated with the Student t test.
To assess the role of cholesterol in endostatin internalization, we resupplied nystatin-treated HUVECs with cholesterol before endostatin incubation. As shown in Figure 1D, nystatin-enhanced endostatin internalization was compromised by cholesterol replenishment in a dose-dependent manner, indicating the involvement of cholesterol in the internalization of endostatin. However, cholesterol alone hardly affected endostatin internalization, possibly because of the existing cholesterol balance on plasma membrane.
Nystatin-enhanced endostatin internalization was further substantiated by flow cytometry. Internalization of Rh-endostatin was increased 1.4- and 2.1-fold by 10 and 25 μg/mL nystatin, respectively (Figure 1E-F). Likewise, amphotericin B, another cholesterol chelator analogous to nystatin, also increased Rh-endostatin internalization in HUVECs (supplemental Figure 2A). Flow cytometric analysis showed that cell-surface binding of endostatin was not apparently elevated by nystatin treatment, ruling out the possibility that nystatin-enhanced endostatin internalization might be because of augmented cell-surface association of endostatin (supplemental Figure 2B-C). In the immunofluorescence assay, internalization of Rh-endostatin was dramatically promoted by nystatin. As shown in Figure 1G and H, the mean fluorescence intensity of Rh-endostatin was increased 2-fold on nystatin treatment. In summary, these results show that endostatin internalization in endothelial cells is significantly enhanced by cholesterol sequestration.
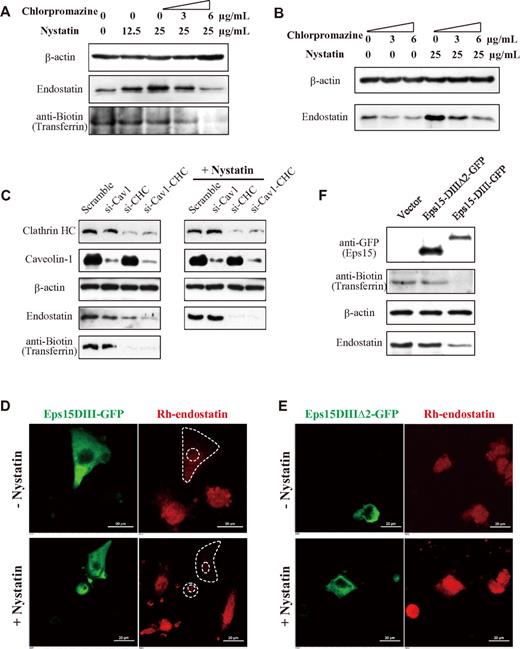
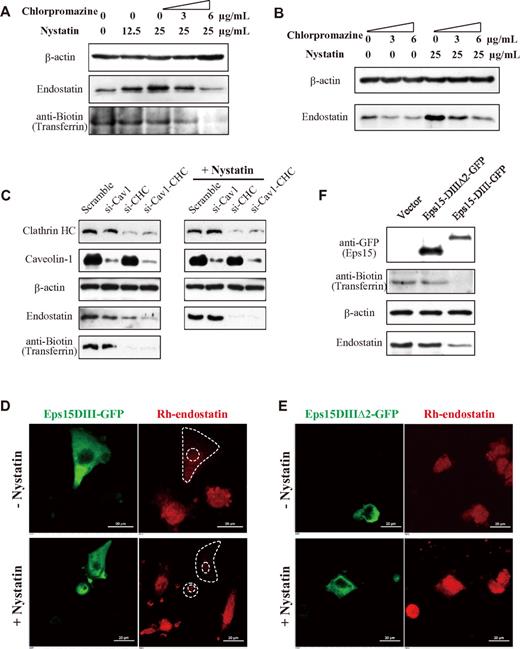
Both caveolae/lipid rafts and clathrin-coated pits are involved in endostatin internalization
Sudhakar et al25 identified integrin α5β1 as one of the endostatin receptors. Integrin α5β1 was found to be internalized through not only clathrin-mediated but also caveolar endocytosis.11-13 Our previous studies established that the angiogenesis-related surface nucleolin functions as another functional receptor of endostatin.24,37 Interestingly, surface nucleolin was also found to associate with lipid rafts and clathrin-dependent internalization.38,39 Given the aforementioned observations, we speculated that endostatin internalization is mediated by both caveolae/lipid rafts and clathrin-coated pits. To investigate the role of clathrin-coated pits in endostatin internalization, we treated the cells with chlorpromazine, an inhibitor of clathrin-coated pit formation,40 combined with nystatin, and then performed endostatin internalization assay. Intriguingly, chlorpromazine dose-dependently compromised nystatin-enhanced endostatin internalization in endothelial cells (Figure 2A). In addition, chlorpromazine alone was able to decrease endostatin internalization (Figure 2B). In contrast, internalization of biotin-labeled transferrin, a marker for clathrin-mediated endocytosis, was dose-dependently abrogated by chlorpromazine but unaffected by nystatin.
Effects of caveolae pathway or clathrin pathway or both pathway inhibition on endostatin internalization in endothelial cells. (A-B) HUVECs were treated with 0, 3, or 6 μg/mL chlorpromazine together with or without nystatin, then applied to endostatin internalization assay. (C) HUVECs were transfected with siRNA against Cav1 (si-Cav1), CHC (si-CHC), or both (si-Cav1-CHC) for 48 hours. Then endostatin internalization was assessed in the absence or presence of nystatin treatment. (D-F) HUVECs were transfected with GFP-tagged Eps15-DIII or wild-type control (Eps15-DIIIΔ2), then treated with 0 or 25 μg/mL nystatin before endostatin incubation. Endostatin internalization was analyzed by immunofluorescence using a Nikon A1 microscope (60×/1.40 NA oil objective) (D-E) and immunoblotting (F). Biotin-transferrin was a marker for clathrin-mediated endocytosis and was detected by the avidin-biotin immunoperoxidase method. Scale bar, 20 μm.
Effects of caveolae pathway or clathrin pathway or both pathway inhibition on endostatin internalization in endothelial cells. (A-B) HUVECs were treated with 0, 3, or 6 μg/mL chlorpromazine together with or without nystatin, then applied to endostatin internalization assay. (C) HUVECs were transfected with siRNA against Cav1 (si-Cav1), CHC (si-CHC), or both (si-Cav1-CHC) for 48 hours. Then endostatin internalization was assessed in the absence or presence of nystatin treatment. (D-F) HUVECs were transfected with GFP-tagged Eps15-DIII or wild-type control (Eps15-DIIIΔ2), then treated with 0 or 25 μg/mL nystatin before endostatin incubation. Endostatin internalization was analyzed by immunofluorescence using a Nikon A1 microscope (60×/1.40 NA oil objective) (D-E) and immunoblotting (F). Biotin-transferrin was a marker for clathrin-mediated endocytosis and was detected by the avidin-biotin immunoperoxidase method. Scale bar, 20 μm.
Knocking down of Cav1 and CHC with the use of specific siRNAs showed that either Cav1 or CHC siRNA prohibited endostatin internalization (Figure 2C). On Cav1 and CHC double knockdown, endostatin internalization was diminished to a larger extent. When treated with nystatin, Cav1 knockdown cells exhibited a similar increase in endostatin internalization comparable to scramble siRNA-transfected cells. One feasible explanation is that, because nystatin treatment largely blocks caveola/lipid raft pathway, nystatin-enhanced endostatin internalization will not be influenced by Cav1 knockdown. Moreover, on nystatin treatment, CHC knockdown (si-CHC and si-Cav1-CHC) cells showed a dramatically abrogated internalization of endostatin, a consequence of the synergistic effects of caveolae/raft inhibition by nystatin plus clathrin pathway inhibition by si-CHC. A second set of siRNAs against Cav1 and CHC were used in parallel to confirm these findings. Consistent results were obtained (supplemental Figure 2D).
To further confirm the participation of clathrin-mediated pathway in endostatin internalization, we overexpressed GFP-tagged Eps15-DIII in HUVECs. Eps15, which binds directly to the adaptor protein AP-2, is essential for the clathrin-mediated endocytosis. Overexpression of Eps15-DIII can selectively sabotage clathrin-mediated endocytosis.30 GFP-tagged Eps15-DIIIΔ2 served as a wild-type control, which had no effect on clathrin-mediated endocytosis. Rh-endostatin uptake was dramatically blocked in those cells efficiently transfected with Eps15-DIII (Figure 2D top). On nystatin treatment, Rh-endostatin uptake was considerably suppressed in Eps15-DIII–transfected cells because of double blockade by nystatin and Eps15 mutant, in marked contrast to the nystatin-enhanced Rh-endostatin uptake by surrounding untransfected cells (Figure 2D bottom). Cells transfected with Eps15-DIIIΔ2 (wild-type control) showed no difference in Rh-endostatin uptake compared with surrounding untransfected cells, in either the nontreated or nystatin-treated condition (Figure 2E). The inhibitory effect of Eps15-DIII on endostatin internalization was also confirmed by immunoblotting (Figure 2F). Together, these results show that inhibition of either caveolae or the clathrin pathway with chemical inhibitors, siRNAs, or dominant-negative mutants alters endostatin internalization, suggesting that both caveolae/lipid rafts and clathrin-coated pits are required for endostatin internalization.
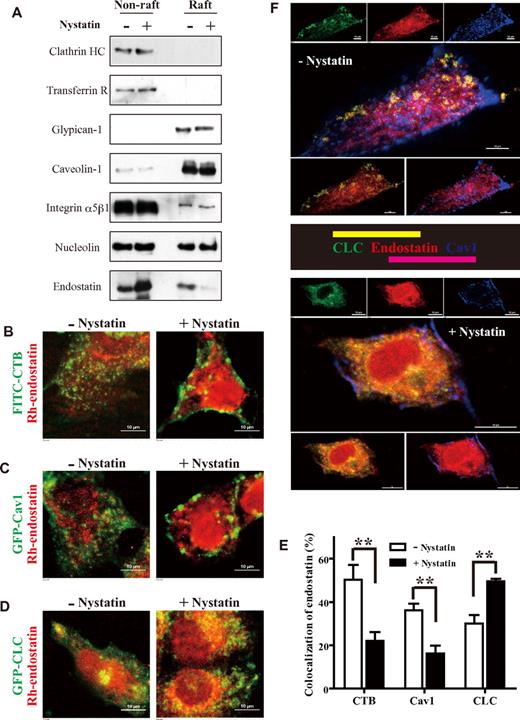
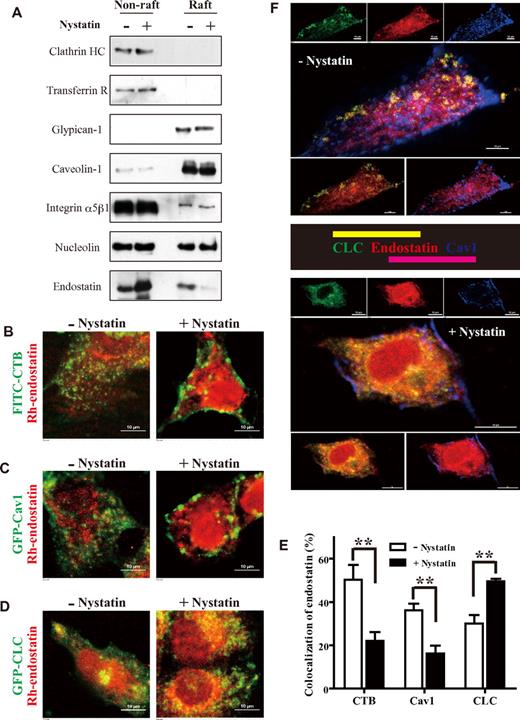
Cholesterol sequestration switches endostatin internalization from caveolae/lipid rafts to clathrin-coated pits
Wickstrom et al27 demonstrated that endostatin associates with Triton-insoluble membrane fraction (lipid rafts) through its interaction with integrin α5β1, GPI-anchored heparan sulfate proteoglycan glypicans, and Cav1. Both filipin III and cyclodextrin treatments block the localization of endostatin in the lipid raft fraction of plasma membrane. However, a large reservoir of endostatin localized to Triton-soluble nonraft fraction is also observed.27 To further assess the localization of endostatin on cholesterol sequestration, whole-cell lysates of HUVECs were separated into Triton-soluble nonraft fraction and Triton-insoluble raft fraction. As shown in Figure 3A, endostatin was present in both raft and nonraft fractions in the absence of nystatin. By contrast, the localization of endostatin in lipid raft fraction was remarkably diminished by nystatin. Interestingly, on nystatin treatment, the distribution of endostatin in nonraft fraction was dramatically increased, indicating a facilitated translocation of endostatin from lipid raft fraction to nonraft fraction. Two previously identified endostatin receptors, nucleolin and integrin α5β1,24,25 were also examined. Nucleolin was found in both raft and nonraft fractions. Integrin α5β1 was predominantly located in nonraft fraction, whereas a small portion of integrin α5β1 in the raft fraction was noticed. By contrast, 2 other endostatin-interacting proteins, Cav1 and heparan sulfate proteoglycan glypican-1, were predominantly in the raft fraction. These observations were concordant with a previous work.27
Nystatin switches endostatin internalization from caveolae/lipid rafts to clathrin-coated pits. (A) HUVECs were treated with 0 or 25 μg/mL nystatin, incubated with 5 μg/mL endostatin at 37°C for 30 minutes, and lysed with 1% Triton X-100 on ice for 30 minutes. Triton X-100 flotation gradients were prepared with a 5%/30%/40% OptiPrep gradient. Clathrin heavy chain (Clathrin HC) and transferrin receptor (Transferrin R) were used as markers for nonraft fractions. Cav1 and glypican-1 were used as markers for raft fractions. (B) HUVECs were treated with 0 or 25 μg/mL nystatin, then incubated with 2 μg/mL FITC-CTB and 5 μg/mL Rh-endostatin at 37°C for 30 minutes. Cells were further fixed and examined by a confocal microscope. (C-D) HUVECs were transfected with GFP-Cav1 or GFP-clathrin light chain (CLC) for 48 hours. Cells were then treated with 0 or 25 μg/mL nystatin and incubated with 5 μg/mL Rh-endostatin at 37°C for 30 minutes. (E) The levels of colocalization (B-D) were quantified by calculating the percentage of red pixels (Rh-endostatin) that colocalized with green pixels (FITC-CTB, GFP-Cav1, or GFP-CLC) from ≥ 8 random fields per well of 3 experiments. (F) Triple fluorescent staining with GFP-CLC (green), Rh-endostatin (red), and anti-Cav1 primary Ab followed by a cyanine 5–conjugated secondary Ab (blue) in the absence or presence of nystatin. Images were obtained using a Nikon A1 microscope (60×/1.40 NA oil objective). Scale bar, 10 μm. **P < .01. Error bars represent SEMs.
Nystatin switches endostatin internalization from caveolae/lipid rafts to clathrin-coated pits. (A) HUVECs were treated with 0 or 25 μg/mL nystatin, incubated with 5 μg/mL endostatin at 37°C for 30 minutes, and lysed with 1% Triton X-100 on ice for 30 minutes. Triton X-100 flotation gradients were prepared with a 5%/30%/40% OptiPrep gradient. Clathrin heavy chain (Clathrin HC) and transferrin receptor (Transferrin R) were used as markers for nonraft fractions. Cav1 and glypican-1 were used as markers for raft fractions. (B) HUVECs were treated with 0 or 25 μg/mL nystatin, then incubated with 2 μg/mL FITC-CTB and 5 μg/mL Rh-endostatin at 37°C for 30 minutes. Cells were further fixed and examined by a confocal microscope. (C-D) HUVECs were transfected with GFP-Cav1 or GFP-clathrin light chain (CLC) for 48 hours. Cells were then treated with 0 or 25 μg/mL nystatin and incubated with 5 μg/mL Rh-endostatin at 37°C for 30 minutes. (E) The levels of colocalization (B-D) were quantified by calculating the percentage of red pixels (Rh-endostatin) that colocalized with green pixels (FITC-CTB, GFP-Cav1, or GFP-CLC) from ≥ 8 random fields per well of 3 experiments. (F) Triple fluorescent staining with GFP-CLC (green), Rh-endostatin (red), and anti-Cav1 primary Ab followed by a cyanine 5–conjugated secondary Ab (blue) in the absence or presence of nystatin. Images were obtained using a Nikon A1 microscope (60×/1.40 NA oil objective). Scale bar, 10 μm. **P < .01. Error bars represent SEMs.
CTB enters cells predominantly via caveola/lipid raft pathway and is widely used as a marker for caveolae/lipid rafts.41 As shown in Figure 3B, Rh-endostatin exhibited colocalization with FITC-conjugated CTB, showed a similarity in endocytic feature between endostatin and CTB in untreated endothelial cells. By disrupting the formation of caveolae, nystatin attenuated the internalization and trafficking of FITC-CTB in nystatin-treated endothelial cells, resulting in a decreased colocalization between Rh-endostatin and FITC-CTB. In comparison, Rh-endostatin internalization was increased by nystatin (Figure 3B right). Similarly, GFP-Cav1 also showed partial colocalization with Rh-endostatin in untreated cells but disturbed colocalization with Rh-endostatin on nystatin treatment (Figure 3C). By contrast, the percentage of Rh-endostatin that colocalized with GFP-clathrin light chain (GFP-CLC) was elevated by nystatin treatment (Figure 3D), which is in agreement with nystatin-promoted localization of endostatin into nonraft fraction (Figure 3A). As shown in Figure 3F, the translocation of endostatin from caveolae/lipid rafts into clathrin-coated pits caused by nystatin was further confirmed with the use of triple-staining confocal microscopy for GFP-CLC, Rh-endostatin, and anti-Cav1. Representative images and quantitative results (Figure 3B-F) showed that endostatin exhibited partial colocalization with both Cav1 and CLC in nontreated endothelial cells. On nystatin treatment, the colocalization levels of endostatin with CTB and Cav1 was decreased by 2.3- and 2.2-fold, whereas intensive colocalization between endostatin and CLC was observed. In summary, these observations show that endostatin is distributed into not only lipid raft but also nonraft fractions in endothelial cells. Cholesterol sequestration with nystatin promotes the translocation of endostatin from caveolae/lipid rafts into clathrin-coated pits and makes the clathrin-mediated pathway the predominant conduit for endostatin internalization, leading to higher uptake efficiency of endostatin in endothelial cells.
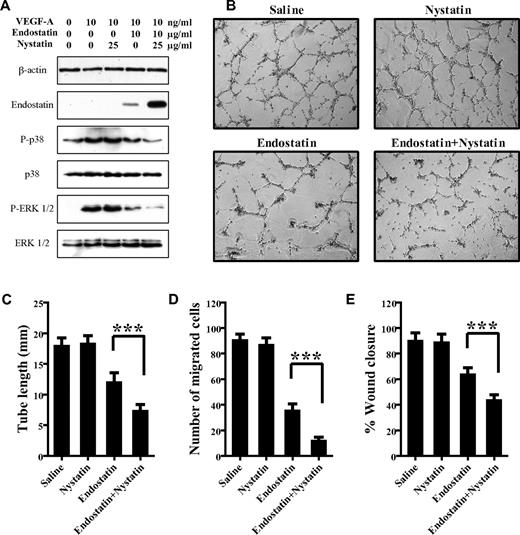
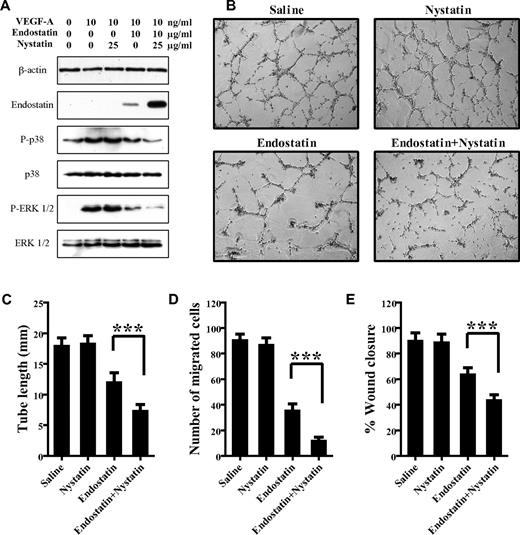
Nystatin increases the inhibitory effects of endostatin on endothelial cell activities
Kim et al42 elucidated the efficacy of endostatin to block VEGF signaling and VEGF-induced rapid p38 MAPK and ERK activation in endothelial cells. To determine whether nystatin-enhanced endostatin internalization leads to an elevated inhibitory efficacy, we assessed the effects of endostatin on VEGF-activated intracellular signaling pathways in the absence or presence of nystatin. As shown in Figure 4A, VEGF dramatically stimulated the phosphorylation and activation of p38 MAPK and ERK1/2. Unsurprisingly, endostatin inhibited VEGF-induced p38 MAPK and ERK1/2 activation. When combined with nystatin treatment, the inhibitory effects of endostatin on VEGF-activated signaling were further increased, possibly because of the promoted internalization and accumulation of endostatin by nystatin in endothelial cells. Nystatin treatment alone had no apparent effect on VEGF-induced p38 MAPK and ERK1/2 phosphorylation, which differs from a previous finding that acute cholesterol depletion (cyclodextrin or progesterone) elevated ERK activation.43 The negligible effect, if any, of nystatin on p38 MAPK and ERK phosphorylation in our study was possibly because of the moderate cholesterol-sequestering condition (25 μg/mL nystatin for 30 minutes) and different responses to cholesterol-binding agents in the presence of VEGF stimulation in endothelial cells.
Nystatin increases the inhibitory effects of endostatin on endothelial cell activities. (A) HUVECs were treated with 0 or 25 μg/mL nystatin, incubated with 0 or 10 μg/mL endostatin for 30 minutes, and then stimulated with 10 ng/mL VEGF 165 for 10 minutes. Phosphorylation levels and basal protein levels of p38 MAPK and ERK1/2 were assessed by immunoblotting. (B-E) HUVECs were treated with saline, 25 μg/mL nystatin, 10 μg/mL endostatin, or a combination of nystatin and endostatin, then measured for tube formation at 6 hours (B-C), transwell migration at 4 hours (D), and the percentage of scratch wound healing at 12 hours (E), respectively. Images from 5 random fields per well of 3 independent experiments were obtained by an optical microscope. ***P < .001. Error bars represent SDs.
Nystatin increases the inhibitory effects of endostatin on endothelial cell activities. (A) HUVECs were treated with 0 or 25 μg/mL nystatin, incubated with 0 or 10 μg/mL endostatin for 30 minutes, and then stimulated with 10 ng/mL VEGF 165 for 10 minutes. Phosphorylation levels and basal protein levels of p38 MAPK and ERK1/2 were assessed by immunoblotting. (B-E) HUVECs were treated with saline, 25 μg/mL nystatin, 10 μg/mL endostatin, or a combination of nystatin and endostatin, then measured for tube formation at 6 hours (B-C), transwell migration at 4 hours (D), and the percentage of scratch wound healing at 12 hours (E), respectively. Images from 5 random fields per well of 3 independent experiments were obtained by an optical microscope. ***P < .001. Error bars represent SDs.
We further investigated whether nystatin promotes the inhibitory efficacies of endostatin on endothelial cell activities in vitro. As shown in Figure 4B and C, tube formation activity of HUVECs was decreased by 34% on endostatin treatment, while being decreased by ≤ 60% on combined treatment with endostatin and nystatin. This difference in tube formation inhibition was considered significant because the inhibitory efficacy of endostatin was almost doubled by nystatin cotreatment. Nystatin alone had no measurable effect on endothelial tube formation activity. Likewise, amphotericin B cotreatment also promoted the inhibitory effect of endostatin on endothelial cell tube formation (supplemental Figure 3A-B). Similarly, in VEGF-induced transwell migration assay (Figure 4D; representative images shown in supplemental Figure 3C), endostatin-treated cells exhibited 50% decrease in trans-migration activity, whereas endostatin plus nystatin cotreated cells exhibited ≤ 80% decrease. A concordant result was also obtained in the scratch wound healing assay (Figure 4E; representative images shown in supplemental Figure 3D). In comparison, the inhibitory effect of angiostatin on endothelial cell transwell migration was not promoted by nystatin (supplemental Figure 4), consistent with the observation that nystatin has no influence on angiostatin internalization (supplemental Figure 1D). In conclusion, these findings show that nystatin cotreatment enhances the inhibitory effects of endostatin on endothelial cell activities.
Nystatin facilitates endostatin uptake by tumors and tumor blood vessels
Fluorescence-labeled endostatin has been shown to selectively distribute in tumors and has been studied as a potential tumor-imaging agent.44 Because our in vitro data implied a strategy to promote endostatin uptake and efficacies with nystatin, we explored whether the uptake and biodistribution of endostatin can be enhanced by nystatin. After intravenous injection of Rh-endostatin together with or without intraperitoneal injection of nystatin, A549 tumors were resected and examined for Rh-endostatin signal with the use of a bioluminescence imaging system. As depicted in Figure 5A and B, nystatin regimen produced a 4.1-fold increase (P < .05) in Rh-endostatin uptake by tumor tissues.
Nystatin facilitates endostatin uptake by tumors and tumor blood vessels. (A-B) Bioluminescence imaging of tumors from A549 tumor–bearing mice treated with 20 mg/kg Rh-endostatin combined with or without 4 mg/kg nystatin. Rh-endostatin fluorescence imaging of excised tumors at 3 hours was shown (n = 4/group). Rhodamine fluorophore excitation (532 nm) and emission (575 nm) filter sets were used. Rh-endostatin signal was quantified as the average fluorescence intensity (B). (C) A549 tumor–bearing mice (n = 4/group) were injected with 125I-endostatin [specific radioactivity, 1 μCi/μg (0.037 Bq/μg); 0.25 mg/kg] combined with or without 4 mg/kg nystatin. 125I-endostatin uptake levels in indicated tissues at 3 hours were calculated as the percentage of the injected dose per gram of tissue wet weight (%ID/g). (D-E) Biotin-endostatin (4 mg/kg) was intravenously injected into A549 tumor–bearing mice combined with or without 4 mg/kg nystatin. Tumors (n = 4/group) were resected at 3 hours and examined by immunofluorescence using a Nikon A1 microscope (20×/0.75 NA air objective). Biotin-endostatin and tumor blood vessels were detected by TRITC-streptavidin and anti-CD31 staining (FITC), respectively. Colocalization percentage of endostatin with CD31 (E) was defined as the area of colocalized biotin-endostatin (red pixels) within CD31-possitive blood vessels (green pixels) divided by the total area of blood vessels. *P < .05 and **P < .01. Error bars represent SEMs.
Nystatin facilitates endostatin uptake by tumors and tumor blood vessels. (A-B) Bioluminescence imaging of tumors from A549 tumor–bearing mice treated with 20 mg/kg Rh-endostatin combined with or without 4 mg/kg nystatin. Rh-endostatin fluorescence imaging of excised tumors at 3 hours was shown (n = 4/group). Rhodamine fluorophore excitation (532 nm) and emission (575 nm) filter sets were used. Rh-endostatin signal was quantified as the average fluorescence intensity (B). (C) A549 tumor–bearing mice (n = 4/group) were injected with 125I-endostatin [specific radioactivity, 1 μCi/μg (0.037 Bq/μg); 0.25 mg/kg] combined with or without 4 mg/kg nystatin. 125I-endostatin uptake levels in indicated tissues at 3 hours were calculated as the percentage of the injected dose per gram of tissue wet weight (%ID/g). (D-E) Biotin-endostatin (4 mg/kg) was intravenously injected into A549 tumor–bearing mice combined with or without 4 mg/kg nystatin. Tumors (n = 4/group) were resected at 3 hours and examined by immunofluorescence using a Nikon A1 microscope (20×/0.75 NA air objective). Biotin-endostatin and tumor blood vessels were detected by TRITC-streptavidin and anti-CD31 staining (FITC), respectively. Colocalization percentage of endostatin with CD31 (E) was defined as the area of colocalized biotin-endostatin (red pixels) within CD31-possitive blood vessels (green pixels) divided by the total area of blood vessels. *P < .05 and **P < .01. Error bars represent SEMs.
To accurately evaluate endostatin uptake levels in tumors as well as normal tissues, we performed 125Iodine-conjugated endostatin tumor uptake experiment in A549 tumor–bearing mice. After intravenous injection of 125I-endostatin with or without intraperitoneal injection of nystatin, selected tissues (blood, heart, liver, spleen, lung, kidney, muscle, and tumor) were resected and counted for radioactivity. As shown in Figure 5C, nystatin cotreatment increased 125I-endostatin uptake (percentage of injected dose per gram) in tumor tissues by 1.4-fold (P < .05). Although kidney is a major organ for urinary excretion of endostatin, nystatin did not elevate the uptake of 125I-endostatin in kidney (P = .11) or any other noncancerous organs of the mice, for that matter. These data indicate that nystatin selectively promotes the uptake and biodistribution of endostatin in tumors but not in healthy organs.
In view of the fact that endostatin is specifically localized to tumor blood vessels,24 we examined whether the uptake of biotin-endostatin in tumor blood vessels is enhanced by nystatin regimen. As depicted in representative images and quantitative illustration (Figure 5D-E), nystatin cotreatment increased the colocalization level of biotin-endostatin within tumor blood vessels by 1.8-fold. In summary, these studies show that combined regimen with nystatin and endostatin dramatically facilitates targeted tumor uptake and tumor blood vessel distribution of endostatin.
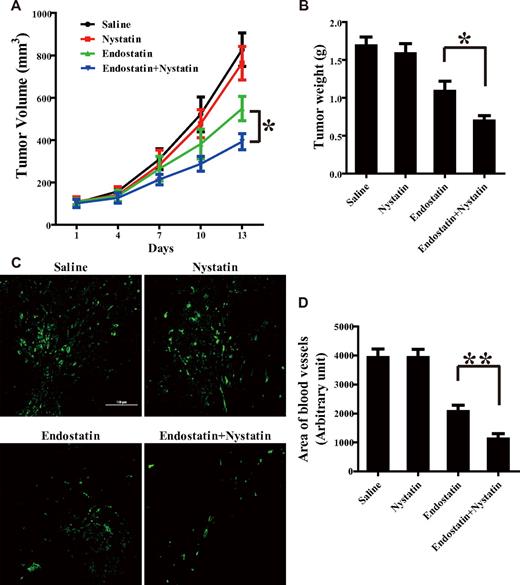
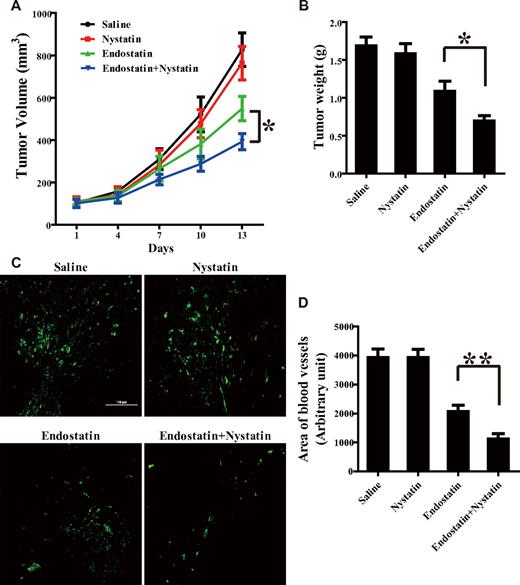
Nystatin enhances the antitumor and antiangiogenic efficacies of endostatin
Because nystatin cotreatment remarkably promotes endostatin uptake by tumor blood vessels and tumor tissues, we further assessed the effects of nystatin regimen on endostatin's antitumor and antiangiogenic efficacies in an A549 xenograft tumor model. A549 tumor–bearing mice received a daily injection of saline, nystatin, endostatin, or a combination of nystatin and endostatin for 14 days. Compared with single-agent treatment with endostatin, combined treatment with nystatin and endostatin further decreased tumor volume by 28% (Figure 6A) and tumor weight by 36% (Figure 6B). Such difference in tumor growth inhibition was considered significant because the inhibitory efficacy of endostatin was almost doubled by nystatin cotreatment.
Nystatin enhances the antitumor and antiangiogenic efficacies of endostatin. When tumor volume reached 0.1 cm3, A549 tumor–bearing mice received daily injections of saline, nystatin (4 mg/kg intraperitoneally), endostatin (4 mg/kg intravenously), or a combination of nystatin and endostatin for 14 days. (A) Tumor volume was measured every 3 days. Tumors (n = 6/group) were resected at 14 days, weighed (B), and applied to immunofluorescent analysis of anti-CD31 blood vessel staining using a Nikon A1 microscope (20×/0.75 NA air objective) (C) and blood vessel area quantification (D). *P < .05 and **P < .01. Error bars represent SEMs.
Nystatin enhances the antitumor and antiangiogenic efficacies of endostatin. When tumor volume reached 0.1 cm3, A549 tumor–bearing mice received daily injections of saline, nystatin (4 mg/kg intraperitoneally), endostatin (4 mg/kg intravenously), or a combination of nystatin and endostatin for 14 days. (A) Tumor volume was measured every 3 days. Tumors (n = 6/group) were resected at 14 days, weighed (B), and applied to immunofluorescent analysis of anti-CD31 blood vessel staining using a Nikon A1 microscope (20×/0.75 NA air objective) (C) and blood vessel area quantification (D). *P < .05 and **P < .01. Error bars represent SEMs.
Nystatin-enhanced antiangiogenic effect of endostatin was also substantiated by monitoring blood vessel density in the same xenograft tumor model (Figure 6C-D). In regard of tumor growth and angiogenesis, nystatin-treated mice displayed no appreciable difference compared with nontreated mice. These results testify that combined treatment with nystatin and endostatin synergistically promotes the antitumor and antiangiogenic activities of endostatin in A549 tumor–bearing mice.
Discussion
Although specific internalization of endostatin into endothelial cells has been extensively observed and proved to be important for the biofunctions of endostatin,18,19,24 the mechanism of its internalization still remains undefined. With the use of several complementary approaches, including pharmacologic inhibitors, siRNAs, and dominant-negative mutants (Figures 1–2), we demonstrate for the first time that internalization of endostatin engages both caveolae/lipid rafts and clathrin-coated pits. Of note, endostatin internalization is dramatically enhanced by cholesterol sequestration, while being decreased by knocking down Cav1. These observations indicate that the caveola/lipid raft functions not only as an essential constituent required for endostatin clustering and internalization but also as a docking platform, which results in a negative contribution to endostatin uptake efficiency. In comparison, the clathrin-mediated pathway serves as a high-efficiency route for endostatin internalization. Thus, cholesterol sequestration by nystatin disrupts caveolae/lipid rafts, attenuates the competition between distinct endocytic pathways, and triggers the translocation of endostatin from the low-efficiency caveolae/lipid rafts to the high-efficiency clathrin-mediated pathway.
Interestingly, in terms of endocytic machinery, endostatin seems to share common features with a variety of cargos, including endothelin receptor type A,5 TGF-β receptors,6 B-cell Ag receptor,7 prion protein,8 bone morphogenetic protein receptor,9 and HM1.24.10 Both caveolae/lipid rafts and clathrin-coated pits are involved in the endocytic process of the aforementioned proteins. In addition, distinct endocytic pathways can be manipulated and switched from one route to another under certain circumstances. For instance, disruption of caveolae/lipid rafts with cholesterol-sequestering agent triggers displacement of prion protein from lipid rafts into clathrin-mediated machinery and elevates its endocytosis in a human neuroblastoma cell line.8
Our results, in conjunction with previous studies, underscore the possibility that the previously identified receptors and interacting proteins of endostatin may function in a correlative pattern. Distinct receptors of endostatin form various combinations and complexes, facilitating endostatin internalization through clathrin pathway or caveolae/lipid rafts or both. Particularly, there is a large reservoir of non–raft-localized integrin α5β1 and nucleolin that can undergo clathrin-mediated endocytosis.13,39 Such non–raft-localized integrin α5β1 and surface nucleolin may mediate the clathrin-dependent internalization of endostatin. Meanwhile, raft-localized endostatin receptors, including integrin α5β1, Cav1, and heparan sulfate proteoglycans, contribute to endostatin association with caveolae/lipid rafts and mediate subsequent internalization of endostatin through the caveola/lipid raft pathway. Interestingly, Sachais et al45 demonstrated that platelet factor 4 diverts the uptake of low-density lipoprotein (LDL) and LDL receptor from the coated pits to the inefficient proteoglycan-dependent endocytic pathway. Nassar et al46 reported that platelet factor 4 markedly promotes the endocytosis and esterification of oxidized LDL. Thrombospondin-1 was also shown to interact with heparan sulfate proteoglycans and LDL receptor–related protein.47 These findings seem to indicate a shared tendency of angiogenesis inhibitors to form complexes and to associate with distinct endocytic pathways. Further investigation of this interesting feature may help elucidate the regulatory mechanisms of these proteins during angiogenesis or other processes such as atherosclerosis and thrombosis.
In contrast to endostatin, the uptake and activity of angiostatin were not affected by nystatin treatment (supplemental Figures 1D and 4), presumably because angiostatin is regulated by a different mechanism from that of endostatin.36 These findings show that nystatin-enhanced endocytosis may not be applicable to all angiogenesis inhibitors. Although it is worth testing more angiogenesis inhibitors such as anginex, thrombospondin, and platelet factor 4, we should consider 2 points: (1) whether the endocytic route of candidate proteins is analogous to that of endostatin and (2) whether the enhanced uptake leads to their promoted activity. For instance, Pilch et al48 reported that internalization is not necessary for the activity of anginex, which compromises the possibility to further promote its activity through enhanced internalization.
Our animal experiments confirm that nystatin selectively increases endostatin uptake and biodistribution in tumor tissues and tumor blood vessels but not in normal tissues. Endostatin can be selectively absorbed in tumors and tumor blood vessels, which is because of the highly expressed endostatin receptors, including integrin α5β1 and cell surface nucleolin, in angiogenic endothelial cells in tumors.24,25,49 Nystatin cotreatment regimen significantly increases endostatin absorption in tumor endothelium, resulting in elevated endostatin uptake by tumor blood vessels and entire tumor tissue. In comparison, endostatin uptake by noncancerous tissues is presumably attributed to nonspecific binding, therefore showing little response to nystatin cotreatment. For example, as the major organ for urinary excretion of endostatin, the kidney shows a high uptake level of endostatin (Figure 5C), which is in accord with the observation of Yang et al.49 However, nystatin cotreatment does not cause an evident increase in endostatin uptake in kidney (P = .11) or in other healthy organs of tumor-bearing mice.
In the Rh-endostatin uptake assay, tumor uptake of Rh-endostatin exhibits a 4.1-fold increase on nystatin cotreatment, compared with a 1.4-fold increase (also statistically significant) in 125I-endostatin uptake assay (Figure 5). The different amplifications are presumably because bioluminescence imaging system detects the Rh-endostatin signal of tumor peripheral area, whereas γ-counter detects the total 125I-endostatin uptake in the entire tumor tissue. Moreover, the various doses of endostatin (20 mg/kg Rh-endostatin vs 0.25 mg/kg 125Iodine-endostatin) in the 2 assays may also influence the fold increase of endostatin uptake by nystatin. These data support our subsequent observation that combined treatment with nystatin and endostatin provides a novel approach to enhance the therapeutic efficacies of endostatin.
Nystatin is used not only as an inhibitor of caveola/lipid raft endocytic pathway in cellular biology, but also as a polyene antifungal drug in human patients. Nystatin can be orally and topically administered in humans or intraperitoneally injected in animals. Although the injectable form of nystatin for human use is not available yet, liposomal nystatin has been extensively studied.50 Our results show that cotreatment with intraperitoneal injection of nystatin remarkably promotes the biodistribution and therapeutic effects of endostatin in tumor-bearing mice. Amphotericin B, another polyene antifungal drug analogous to nystatin, also evidently enhances the uptake and inhibitory effects of endostatin in parallel experiments (supplemental Figures 2-3). In addition, soluble amphotericin B can be intravenously administered, whereas intravenous liposomal nystatin is being tested in clinical trials, showing a potential drug combination of endostatin with amphotericin B, in addition to nystatin.
Because recombinant human endostatin has been approved by the State Food and Drug Administration of China for the treatment of non–small cell lung cancer, it is intriguing to further evaluate whether the combined treatment with endostatin and nystatin could enhance endostatin efficacy in clinical studies. In addition, cholesterol sequestration may also regulate the uptake of other proteins whose internalization is similarly mediated by caveolae/lipid rafts and clathrin. The candidate list may include not only the angiogenesis inhibitors but also other functional proteins that are internalized by different cell types. If this is the case, our combined regimen may open a new avenue toward efficient delivery of drugs that include (but are not limited to) antiangiogenesis molecules. Intriguingly, one of our ongoing projects shows that the uptake and biodistribution of some monoclonal Abs that target tumor cells are also enhanced by nystatin cotreatment, supporting the notion that this combined regimen may have broader application in cancer therapeutics.
In conclusion, our study shows that endostatin internalization is mediated by both caveolae/lipid rafts and clathrin-coated pits. Cholesterol sequestration by nystatin switches endostatin translocation from the low-efficiency caveolae/lipid rafts to the high-efficiency clathrin-mediated pathway, resulting in promoted internalization and biofunctions of endostatin in endothelial cells. Furthermore, tumor-specific uptake and antiangiogenic and antitumor efficacies of endostatin are also dramatically enhanced by the combined treatment with nystatin. This study, for the first time, points out the possibility that cholesterol sequestration may provide a novel route to enhance the uptake and efficacy of endostatin via regulating distinct endocytic pathways.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Du Feng (Tsinghua University) and Alexandre Benmerah (Cochin Institute) for providing plasmids; Fan Wang, Bing Jia, and Sujuan Yang (Peking University) for iodine-labeling experiment; Jing Bai and Fei Liu (Tsinghua University) for fluorescence imaging; and members of the Luo laboratory for insightful discussions.
This work was supported in part by the General Programs of the National Natural Science Foundation of China (no. 30771083), the National High Technology Research and Development Program of China (no. 2007AA02Z155 and no. 2008AA02Z136), and the National Science & Technology Major Project (no. 2009ZX09103-703 and no. 2009ZX09306-002).
Authorship
Contribution: Y.C. designed and conducted research and wrote the paper; S.W., X.L., H.Z., and Y.F. conducted research and analyzed data; and Y.L. designed research, analyzed data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Yongzhang Luo, School of Life Sciences, Tsinghua University, Beijing 100084, China; e-mail: yluo@tsinghua.edu.cn.

![Figure 5. Nystatin facilitates endostatin uptake by tumors and tumor blood vessels. (A-B) Bioluminescence imaging of tumors from A549 tumor–bearing mice treated with 20 mg/kg Rh-endostatin combined with or without 4 mg/kg nystatin. Rh-endostatin fluorescence imaging of excised tumors at 3 hours was shown (n = 4/group). Rhodamine fluorophore excitation (532 nm) and emission (575 nm) filter sets were used. Rh-endostatin signal was quantified as the average fluorescence intensity (B). (C) A549 tumor–bearing mice (n = 4/group) were injected with 125I-endostatin [specific radioactivity, 1 μCi/μg (0.037 Bq/μg); 0.25 mg/kg] combined with or without 4 mg/kg nystatin. 125I-endostatin uptake levels in indicated tissues at 3 hours were calculated as the percentage of the injected dose per gram of tissue wet weight (%ID/g). (D-E) Biotin-endostatin (4 mg/kg) was intravenously injected into A549 tumor–bearing mice combined with or without 4 mg/kg nystatin. Tumors (n = 4/group) were resected at 3 hours and examined by immunofluorescence using a Nikon A1 microscope (20×/0.75 NA air objective). Biotin-endostatin and tumor blood vessels were detected by TRITC-streptavidin and anti-CD31 staining (FITC), respectively. Colocalization percentage of endostatin with CD31 (E) was defined as the area of colocalized biotin-endostatin (red pixels) within CD31-possitive blood vessels (green pixels) divided by the total area of blood vessels. *P < .05 and **P < .01. Error bars represent SEMs.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/117/23/10.1182_blood-2010-12-322867/4/m_zh89991172020005.jpeg?Expires=1767732308&Signature=fRPOCYzNniYVyOOB4tshqSDr4t2jmgmelpCFstdNPnJ4XBrRiOpTGn1Uc-~BruwA3BHg99y67vFjSWCg78zpHTIM6EWJfTTh~B7C8Xz-W1DlHuI~LJ3LoXQdYRsL1H6IJ7mvyMNvuNcGkuhhpvWLsMwzA9BKLGXU-9qZgRFd6JJ6~LDTSDjRKBxA96slOIBf7-qCHIZbyt6q7n~yynOX2w5E7v7vAJaAI-bChJsXGgV1ovJNB4Hwy5YnxeNbU633WBc0~Npu3tro2j6nCMHHLhqY8sEFo6AQcR~AjVu35xA5GODAddWwbtxoeVF8PK347p5HRHMem~SdGLyX--v~CA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

![Figure 5. Nystatin facilitates endostatin uptake by tumors and tumor blood vessels. (A-B) Bioluminescence imaging of tumors from A549 tumor–bearing mice treated with 20 mg/kg Rh-endostatin combined with or without 4 mg/kg nystatin. Rh-endostatin fluorescence imaging of excised tumors at 3 hours was shown (n = 4/group). Rhodamine fluorophore excitation (532 nm) and emission (575 nm) filter sets were used. Rh-endostatin signal was quantified as the average fluorescence intensity (B). (C) A549 tumor–bearing mice (n = 4/group) were injected with 125I-endostatin [specific radioactivity, 1 μCi/μg (0.037 Bq/μg); 0.25 mg/kg] combined with or without 4 mg/kg nystatin. 125I-endostatin uptake levels in indicated tissues at 3 hours were calculated as the percentage of the injected dose per gram of tissue wet weight (%ID/g). (D-E) Biotin-endostatin (4 mg/kg) was intravenously injected into A549 tumor–bearing mice combined with or without 4 mg/kg nystatin. Tumors (n = 4/group) were resected at 3 hours and examined by immunofluorescence using a Nikon A1 microscope (20×/0.75 NA air objective). Biotin-endostatin and tumor blood vessels were detected by TRITC-streptavidin and anti-CD31 staining (FITC), respectively. Colocalization percentage of endostatin with CD31 (E) was defined as the area of colocalized biotin-endostatin (red pixels) within CD31-possitive blood vessels (green pixels) divided by the total area of blood vessels. *P < .05 and **P < .01. Error bars represent SEMs.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/117/23/10.1182_blood-2010-12-322867/4/m_zh89991172020005.jpeg?Expires=1767732309&Signature=RzjCOoQUg922oXVEkA~CEUvymS0Nkhs6pZFzds58JOzM2LBjUlJl65v2~a6C2TGmSZ1Rx2TF5Xm4Wf99GOHLA~4LmXmgSMupKTTlCfxoEc8g1r3sEIJqkwuUaWUSJYBOdbdn3i3USKlqKXWjw1UAQkwPAybpv-qQXS6p9iYRPo0edIiS6mpX0~0PAfb9wf4TbA4EJXclIFqCW9X75NQVB98kaJ3Fbk~TU~zXn6gHQAvBSWZV5EdVCKuXLTpKH6cnZvi4pIB6aPw9MixMLYiG~xLOlDjhXc-Ld5Zdp2GchD8GZEhcubm1sWX8V6jEHzaVfCgQNamRXs6efNNCi~5kCg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)