Human herpesvirus 6 (HHV-6) is recognized as a sporadic cause of encephalitis in hematopoietic cell transplantation (HCT) recipients. In this issue of Blood, Zerr and coworkers report on a 3.5-year prospective study of 315 patients undergoing allogeneic HCT.1 Patients with HHV-6 were more likely to develop delirium and neurocognitive decline. The results support a future clinical trial to test whether antiviral prophylaxis will reduce CNS morbidity after HCT.
Any physician who cares for patients undergoing HCT can describe the feeling of helplessness that comes over the medical care team as a patient descends into an episode of encephalitis, which for many leads to death or permanent disability despite antiviral therapy. Thankfully, it is not a common event. In this issue of Blood, Zerr and colleagues report the results of a large, well-controlled, prospective study of patients undergoing HCT. Their results temporally link HHV-6 reactivation in the peripheral blood and more common CNS dysfunction, including delirium during the early after-transplantation period and neurocognitive decline measured 12 weeks after transplantation.1 The finding that HHV-6 is a major cause of delirium and impaired neurocognitive function in HCT recipients confirms and extends previous studies on the connection between HCT, reactivation of HHV-6, and encephalitis.2-4
Although encephalitis is often considered the most severe form of CNS dysfunction, the present study suggests that delirium is a clinically meaningful end point because of its association with impaired cognitive function and diminished quality of life 1 year after transplantation.5 In addition, delirium and neurocognitive function can be objectively measured using well-validated instruments, highlighting the utility of these outcomes in future studies of CNS disease associated with HHV-6. The study by Zerr et al also identifies more advanced underlying disease as a risk for an episode of delirium associated with HHV-6 and confirms previously reported variables associated with HHV-6 reactivation after HCT: cord blood or unrelated cell source. Although previous smaller studies have not found the type of conditioning regimen to affect reactivation, the present study did find that reduced intensity conditioning was a risk factor as well.
Prior reports of HCT and HHV-6 have suggested a link between the viral load measured in plasma or peripheral blood mononuclear cells and the development of disease.2-4 The present study confirms this association by demonstrating an increased odds ratio for neurocognitive decline in subjects with HHV-6 viral loads > 1000 copies/mL of plasma.
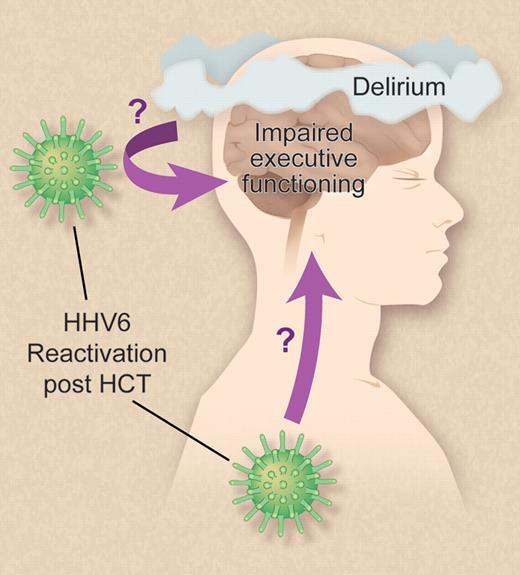
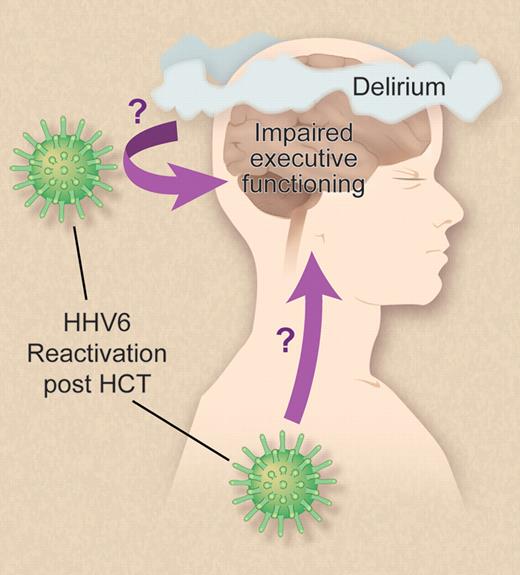
Several important questions remain. First, it is not clear whether HHV-6 reactivates within the CNS as well as in the periphery (see figure), and if so, whether reactivation is selective to particular brain regions or cell types. The available data suggest partial and conflicting answers. In a small group of patients with HHV-6 encephalitis after HCT the viral loads in cerebrospinal fluid (CSF) were much greater (2 log10) than in children with encephalitis/encephalopathy during primary infection, suggesting local reactivation in the CNS.6 Autopsy studies of 3 patients who died after HHV-6–associated encephalitis have demonstrated active infection of brain tissue via detection of viral DNA, RNA, and proteins also suggesting local replication.7 Yet in this report by Zerr and colleagues only 2 of 4 subjects with delirium associated with HHV-6 reactivation had viral DNA detected in the CSF. It is possible that HHV-6 reactivation in either the periphery or the CNS may induce disease, or that transient reactivation in the CNS may be sufficient to elicit neurocognitive sequelae.
Zerr et al show that HHV-6 reactivation post-HCT is associated with increased risk of delirium and neurocognitive decline, marked by selective impairment of executive functioning with relative sparing of memory and fine motor skills.1 Still unresolved is the question of whether HHV-6 reactivates locally within the CNS as well as in the periphery, and whether virus reactivation within the CNS is required for viral effects on cognitive function. Professional illustration by Debra Dartez.
Zerr et al show that HHV-6 reactivation post-HCT is associated with increased risk of delirium and neurocognitive decline, marked by selective impairment of executive functioning with relative sparing of memory and fine motor skills.1 Still unresolved is the question of whether HHV-6 reactivates locally within the CNS as well as in the periphery, and whether virus reactivation within the CNS is required for viral effects on cognitive function. Professional illustration by Debra Dartez.
This leads to an additional question: How is HHV-6 causing delirium? Is it the direct consequence of viral infection of CNS cells or an indirect effect of virally induced (neuro)inflammation? Two recent reports have linked proinflammatory cytokines (IL-6) in plasma and CSF to CNS disease in both HCT recipients and children with primary HHV-6 infection.4,6 However, the association between HHV-6 viral loads and the risk of CNS dysfunction after HCT, as well as the temporal relationship between HHV-6 reactivation and CNS disease, argues for a more direct effect of virus replication. Direct virally induced CNS damage may also explain why delirium has durable consequences in HCT recipients.
The brain region(s) affected by HHV-6 reactivation in HCT recipients are unknown, but the clinical presentation reported by Zerr and coworkers reveals selective loss of executive function (attention, processing speed, concentration, and cognitive flexibility) with sparing of memory (both verbal and visual) and fine motor skills. This profile is a little unexpected, given previous reports that HHV-6 infection is principally associated with the hippocampus and amygdala, at least in cases of limbic encephalitis.8
Ultimately the most pressing question raised by the present research is this: Would HCT recipients benefit from prophylaxis to prevent early reactivation of HHV-6? Three very small trials using ganciclovir prophylaxis reported a decrease in HHV-6 reactivation in treated patients,9-11 while a recent report of a preemptive strategy did not demonstrate any benefit.12 Because of the myelosuppressive effects of ganciclovir and the failure of preemptive ganciclovir treatment, the use of foscarnet in an HHV-6 prophylaxis study has been suggested.12 However, the drawbacks of foscarnet (intravenous administration, electrolyte disturbances, and renal dysfunction) lead to a narrow risk benefit calculation and limit the practical use of this drug for prophylaxis. An alternative may be the lipid-ester derivative of cidofovir, hexadecyloxypropyl-cidofovir (CMX001). This compound has broad activity against DNA viruses, can be administered orally with little toxicity, and has been detected in the CSF after administration.13
Although a perfect antiviral drug may not be available, we agree with Zerr et al that the time has come to perform a randomized, double-blind, controlled, prophylaxis trial to determine definitively if the prevention of HHV-6 reactivation reduces CNS disease in HCT patients, so that we can all emerge from our confusion.
Conflict-of-interest disclosure: The authors declare no competing financial interests. ■