Abstract
The anti-CD20 monoclonal antibody (mAb) rituximab has revolutionized the treatment of B-cell malignancies. This unprecedented success has not only substantially changed the mindset of the clinical community about the ability of mAb to improve outcomes but has catalyzed the interest in the pharmaceutical industry to develop the next generation of anti-CD20 mAbs. Since the introduction of rituximab 15 years ago, we have learned much about the potential mechanisms underlying the therapeutic efficacy of anti-CD20 mAbs. In parallel, many novel anti-CD20 mAbs have entered the clinic, each designed with modifications to structure aimed at further improving efficacy. On review of the newer generation of anti-CD20 mAbs entering clinical trials, it appears that the link between the novel mechanistic insights and the development of these next-generation anti-CD20 mAbs is unclear. As we move into an era of personalized medicine, it will become increasingly important for us to develop closer links between the emerging mechanistic insights and the clinical development, to further enhance the potency of anti-CD20 mAbs beyond that achieved with rituximab.
Introduction
The advent of monoclonal antibody (mAb) technology after the Nobel Prize–winning scientific contribution of Kohler and Milstein1 led to a great expectation that mAbs would provide effective targeted therapy for cancer. After early promise came a period of despondency in the late 1980s and early 1990s with largely disappointing early phase clinical trial results, with the notable exception of anti-idiotype antibodies in follicular lymphoma (FL).2,3 More than 20 years elapsed before mAbs began to fulfill their early promise as effective anticancer therapeutics, and many lessons were learned from these clinical trial failures. When the first successes were seen in hematologic malignances, the importance of the antigen target specificity and developing “humanized” mAbs was recognized. In hematologic malignancies, the major success of mAb therapy to date has been seen with anti-CD20 mAbs. Although the first B cell–specific antibody B1 (renamed tositumomab), which targets the B cell–specific antigen that we now know as CD20, was discovered as long ago as 1981,4 it was not until 1997 that the anti-CD20 rituximab became the first mAb to be approved by the U.S. Food and Drug Administration (FDA) for use in relapsed indolent lymphoma.5 mAbs are now routinely delivered in a wide range of hematologic malignancies, and rituximab is widely accepted to be the single most important factor leading to improved outcome in a range of B-cell lymphomas6-10 and more recently in B-cell chronic lymphocytic leukemia (B-CLL).11,12
As we reflect on the development of rituximab in the late 1990s, there were considerable challenges and uncertainties for those early pioneers to overcome in integrating rituximab into treatment protocols. Given those difficulties, much of what has now become standard practice was the result of serendipity and pragmatism rather than the application of high-quality translational science. This is well illustrated, for example, by the initial scheduling and dosing of rituximab at 375 mg/m2 weekly for 4 doses that became established and licensed. This same dose of 375 mg/m2 subsequently became the dose given 3 times weekly with combination chemotherapy in B-cell lymphoma to all patients regardless of factors known to affect pharmacokinetics, such as tumor burden, and is not adjusted according to serum rituximab levels.13
Despite the unprecedented success of rituximab, a proportion of patients with CD20 positive malignancies still fail to respond to, or more commonly relapse, after receiving rituximab-containing immunochemotherapy. As we look to the future, we can be certain that the optimal treatment approach for such “rituximab-refractory” patients will play an ever-increasing part of the clinical challenge for B-cell malignancies. The current challenge lies in providing effective therapies for those patients who develop resistance to rituximab. Although it is approaching 30 years since the discovery of CD20 and tositumomab, there remains much that we continue to learn about anti-CD20 mAb effector mechanisms. These new insights may prove relevant to further unlocking the potential of anti-CD20 mAbs to improve clinical outcomes. The interest in anti-CD20 mAb continues to provide a major focus for scientific and clinical investigators alike, and it seems highly probable that this research interest will continue to grow as the next generation of anti-CD20 mAbs is developed and tested in the clinic. The unparalleled successes of rituximab along with the rapid development of mAb engineering technology have fueled intense investigation into the development of a new generation of anti-CD20 mAbs by the pharmaceutical industry. Each of these new mAbs attempts to further improve therapeutic efficacy (see Table 1). As we survey the many new tools now arriving in the physician's tool kit, it is timely to ask the question as to whether and how these tools differ from each other and, most importantly, whether any of them will provide additional therapeutic benefits over that achieved with rituximab.
In this Perspective, we critically address 2 important questions regarding the burgeoning development of new anti-CD20 mAb: (1) Are we are truly exploiting the new scientific insights into mechanism of action with appropriate rationale for novel anti-CD20 mAb design? (2) What is the likelihood of these newly developed anti-CD20 mAb to improve clinical efficacy in B-cell malignancies over the existing standard of rituximab?
What have we learned about how anti-CD20 mAbs work?
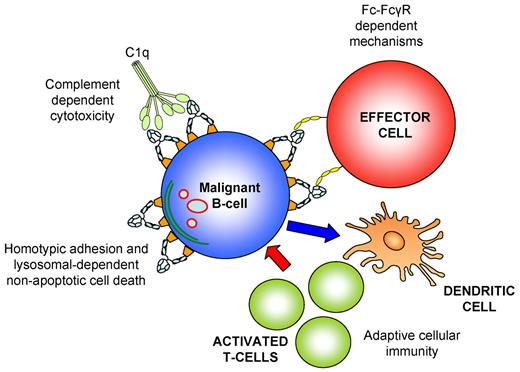
Before addressing these 2 questions, it is pertinent to look back and review what we have learned about the mechanisms of action of anti-CD20 mAb. Certainly, when rituximab was first used in the clinic, there was much uncertainty as to the mechanisms underlying clinical responses. Although some uncertainty still remains, we have discovered many new insights over the last decade into how anti-CD20 mAb contributes to tumor clearance. Anti-CD20 mAbs appear to eliminate their targets by engaging in a range of effector pathways. These include mAb Fc-FcγR interactions, including antibody-dependent cellular cytotoxicity (ADCC) and phagocytosis, complement-dependent cytotoxicity (CDC), and the direct induction of programmed cell death (PCD).14 More recently, evidence has emerged to suggest a potential role for passive antibody induced immunization14 (Figure 1).
Potential anti-CD20 mAb effector mechanisms. (A) Fc-FcγR–dependent mechanisms. The Fc arm of anti-CD20 mAb recruits and activates FcγR-expressing immune effector cells, including macrophages and NK cells, which in turn eliminate the target cell by release of cytotoxic mediators in ADCC (NK cells and macrophages) or direct phagocytosis (macrophages). (B) CDC. Complement fixation occurs when C1q, the globular head of C1, binds the Fc portion of 2 IgG molecules, which triggers a series of enzymatic reactions that generate pores in the cell membrane (membrane attack complex) leading to cell lysis. (C) Direct PCD is induced primarily by type II anti-CD20 mAbs through an actin-dependent, lysosomal pathway after homotypic adhesion. (D) Adaptive cellular immunity. Anti-CD20 mAbs promote the uptake of tumor antigens by dendritic cells and cross-presentation to T cells, which differentiate into cytotoxic T cells that evoke an antitumor cellular immune response.
Potential anti-CD20 mAb effector mechanisms. (A) Fc-FcγR–dependent mechanisms. The Fc arm of anti-CD20 mAb recruits and activates FcγR-expressing immune effector cells, including macrophages and NK cells, which in turn eliminate the target cell by release of cytotoxic mediators in ADCC (NK cells and macrophages) or direct phagocytosis (macrophages). (B) CDC. Complement fixation occurs when C1q, the globular head of C1, binds the Fc portion of 2 IgG molecules, which triggers a series of enzymatic reactions that generate pores in the cell membrane (membrane attack complex) leading to cell lysis. (C) Direct PCD is induced primarily by type II anti-CD20 mAbs through an actin-dependent, lysosomal pathway after homotypic adhesion. (D) Adaptive cellular immunity. Anti-CD20 mAbs promote the uptake of tumor antigens by dendritic cells and cross-presentation to T cells, which differentiate into cytotoxic T cells that evoke an antitumor cellular immune response.
The relative contribution of each of these mechanisms appears to be at least partially dependent on the mouse model and type of anti-CD20 mAb used.15-18 Cragg et al initially characterized anti-CD20 mAbs into 2 subtypes based on their ability to redistribute CD20 in membrane lipid rafts. Type I “rituximab-like” anti-CD20 mAbs redistribute CD20 into membrane lipid rafts and potently activate complement,19 whereas type II anti-CD20 mAbs, such as tositumomab, weakly activate complement but more potently evoke direct PCD.20-22 Both subtypes show equal ability in activating FcγR-bearing immune effector cells.15,23
Are FcγR-expressing immune effector cells the key to unlocking the therapeutic efficacy of anti-CD20 mAb?
Current evidence indicates that Fc-FcγR–dependent mechanisms are perhaps the most critical for the efficacy of anti-CD20 mAbs. This was first demonstrated by Clynes et al who showed that rituximab therapy in a lymphoma xenograft model was completely dependent on activatory FcγR.24 More recently, syngeneic mouse models using antimouse CD20 mAbs demonstrated that activatory FcγR were required for the depletion of normal B cells18,25 as well as adoptively transferred primary murine lymphoma.26 Clinical studies in FL patients appear to corroborate these preclinical findings in which rituximab-treated patients who carry genetic polymorphisms of FcγRIIIa (CD16) with a high affinity for IgG (158 V/V) have a higher progression-free survival, compared with patients with low-affinity polymorphisms (158 F/F or 158 V/F).27 In contrast, studies examining the role of FcγR-polymorphisms in predicting the clinical outcome using immunochemotherapy are conflicting. Some studies conclude that such polymorphisms predict response to immunochemotherapy, but not chemotherapy alone in diffuse large B-cell lymphoma (DLBCL)28 and FL,29 whereas other studies examining cyclophosphamide, doxorubicin, vincristine, prednisone with rituximab (R-CHOP)–treated DLBCL30 and FL31 populations reported no association. In CLL, FcγR polymorphisms failed to predict the response to rituximab alone32 or in combination with chemotherapy.33 This observation may potentially be explained by the impaired function of innate immune effector cells observed in CLL patients.34 It also suggests that Fc-FcγR interactions may not be the dominant mechanism of action of anti-CD20 mAbs in CLL therapy and that other effector mechanisms may be more important in different B-cell malignancies. Clearly, further large prospective studies are required to determine whether the importance of FcγR-polymorphisms in predicting clinical outcome varies across different patient populations and treatment combinations.
The precise nature of the FcγR-expressing effector cell population responsible for the therapeutic effect of anti-CD20 mAbs remains the subject of much debate. Anti-CD20 mAbs have been shown to activate natural killer (NK) cells, macrophages, and neutrophils to eliminate B cells in vitro.15,35,36 In contrast to these in vitro observations, there is now substantial preclinical evidence from mouse models indicating that macrophages are the key immune effector cells required for the therapeutic effect of anti-CD20 mAbs in vivo, with no demonstrable role for neutrophils or NK cells.16,18,37,38 Correlative clinical studies also appear to support these preclinical in vivo data in suggesting that macrophages may play an important role in rituximab therapy. Two clinical studies have demonstrated that rituximab appears able to circumvent the poor prognostic signature of high tumor-associated macrophage (TAM) content, implying that rituximab may recruit macrophages to improve outcome. Taskinen et al initially showed that high TAM content predicted a favorable outcome in FL patients treated with immunochemotherapy (R-CHOP).39 Subsequently, in a larger study, Canioni et al demonstrated that a high TAM content was associated with poor outcome in FL patients treated with chemotherapy and interferon, but not in those receiving rituximab plus chemotherapy and interferon.40 The authors suggested that rituximab can circumvent this previously established unfavorable prognosis of high TAM counts.40 Weng and Levy27 also showed that polymorphisms of FcγRIIa (CD32), which is expressed predominantly on macrophages, and only a small subset (3%-7%) of NK cells,41 can also predict outcome after treatment with rituximab in FL. Although these clinical studies suggest a potential role for macrophages in rituximab therapy, it is important to note that they are correlative and do not exclude the contribution of other FcγR-expressing effector cells, such as NK cells and neutrophils which have also been implicated in humans.35,36
Is complement a friend or foe?
Although the contribution of complement to the therapeutic efficacy of anti-CD20 mAb remains disputed, recent data suggest that complement is not an important component for clearance of tumor15,18,26 and may indeed even be detrimental to therapeutic efficacy.42 There is no doubt that rituximab does effectively engage C1q and induces CDC in lymphoma cell lines and primary tumor cells in vitro because of its ability to rapidly redistribute CD20 into membrane lipid rafts.19,43 The importance of this mechanism in the elimination of B cells in vivo does, however, remain controversial. Complement appears to be required for rituximab therapy in mouse models in which the mAb does not cross-react with the normal host B-cell reservoir.16,17,44 In contrast, studies in fully syngeneic mouse models have shown that complement is not required for the therapeutic effect of anti-CD20 mAb. Importantly, depletion of normal and malignant B cells using antimouse CD20 mAb was equally effective in C1q- and C3-deficient mice compared with wild-type mice.18,26 In a human CD20 (hCD20) transgenic mouse model, B-cell depletion by a rituximab variant that does not engage C1q was also equally effective in B-cell depletion compared with wild-type rituximab.15 Furthermore, although complement is rapidly consumed after rituximab administration in patients,45 the expression of the complement defense proteins CD55 and CD59 on the surface of malignant B cells did not predict the clinical outcome of rituximab treatment in FL,46 nor did CD59 expression in B-CLL,47 suggesting that CDC is unlikely to play a substantial role in the therapeutic effect of rituximab.
Several reports have suggested that complement activation by anti-CD20 mAbs may have deleterious effects. Complement activation was shown to play a key role in the toxicity related to the infusion of mAbs in animal models48 ; and in a small clinical study, complement activation was found to correlate with the infusional toxicity of rituximab.49 More recently, Wang et al proposed that complement can be detrimental to anti-CD20 mAb therapy by showing that complement activation inhibits rituximab-induced ADCC and NK-cell activation50 and that complement depletion enhances rituximab-induced NK-cell activation and improves mAb therapeutic efficacy in a syngeneic mouse model, although the latter was demonstrated with an anti-idiotype mAb and not rituximab.42 This hypothesis is corroborated in a clinical study of FL patients in which a C1qA polymorphism associated with low C1q levels correlated with a prolonged response to rituximab.51 Further studies are required to confirm whether the prolonged responses observed are the result of the lack of complement activation, as C1q has diverse immunologic functions in addition to the initiation of the complement cascade.51 Overall, although the detrimental role of complement in anti-CD20 mAb therapy requires further substantiation, these studies suggest that a focus on improved CDC is unlikely to significantly augment the efficacy of anti-CD20 mAbs.
Can we improve antitumor responses further by inducing direct antibody-induced cell kill?
An interesting and relatively underexplored mechanism of action of anti-CD20 mAbs is the induction of direct mAb-induced PCD on antigen ligation. In vitro studies have demonstrated that rituximab can induce apoptotic cell death in malignant B cells, which was dependent on hyper-crosslinking rituximab with agents, such as antihuman IgG.52-55 These types of studies may not represent optimal models to simulate potential rituximab cross-linking in vivo, which presumably occurs through FcγR-bearing effector cells.20 Furthermore, de Haij et al have shown that such PCD-dependent on cross-linking does not contribute to tumor depletion by rituximab in vivo.56 In contrast, Byrd et al have demonstrated that rituximab induces caspase activation in a cohort of CLL patients, which correlates with tumor cell depletion.57 The mode of apoptosis induction, however, is undetermined and could be mediated directly by mAb or indirectly through FcγR-expressing effector cells. Because the ability of rituximab to mediate direct PCD without extensive cross-linking appears limited, some investigators postulate that rituximab exerts its direct effect through sensitizing tumor cells to chemotherapy-induced apoptosis. Bonavida et al demonstrated that rituximab chemosensitizes lymphoma cell lines in vitro by down-regulating the antiapoptotic proteins BCL-2 and BCL-XL through the inhibition of various signaling pathways, including p38 mitogen-activated protein kinase, NF-κB, and Akt,58-60 and can increase chemotherapy-induced apoptosis in vivo.61 Interestingly, long-term follow-up of one of the early phase 2 trials using R-CHOP in FL revealed that 7 of the 8 patients who were BCL-2 positive at baseline, subsequently became BCL-2-negative.62 Two independent retrospective analyses of clinical studies in DLBCL demonstrated that the addition of rituximab to chemotherapy significantly improved overall survival over chemotherapy alone in patients with BCL-2-positive tumors, but not BCL-2-negative tumors, suggesting that patients with BCL-2-positive DLBCL have derived greater benefit from rituximab.63,64 Whether this increased benefit is the result of the ability of rituximab to down-regulate BCL-2 in BCL-2–overexpressing primary tumors is yet to be determined, as contrary to lymphoma cell lines, evidence to suggest that rituximab alters the expression of BCL-2 in primary tumor cells is currently lacking.57
In contrast to type I anti-CD20 mAb, such as rituximab, type II anti-CD20 mAbs appear more potent in inducing PCD but are currently underexplored in the clinic. Tositumomab is the only type II anti-CD20 mAb, which is FDA-approved as part of the Bexxar radioimmunotherapy regimen. This radioimmunotherapy is highly effective in FL patients refractory to both chemotherapy65 and rituximab.66 Type II anti-CD20 mAbs have been shown to induce nonapoptotic PCD that it is independent of BCL-2 and caspases20 or the induction of DNA double-strand breaks.20,22 Cell death was triggered through an Fc-independent manner, as F(ab′)2 fragments were sufficient for PCD induction.16,22,67
Type II anti-CD20 mAbs have also been found to be more effective at prolonging survival than rituximab or other type I anti-CD20 mAbs in lymphoma xenograft models.16 Importantly, treatment with F(ab′)2 fragments of type II, but not type I, anti-CD20 mAbs resulted in substantial improvements in survival, suggesting that Fc-independent mechanisms may indeed contribute to the enhanced therapeutic efficacy of type II anti-CD20 mAbs.16 Type II anti-CD20 mAbs were also more effective at depleting normal B cells compared with rituximab in a syngeneic hCD20 transgenic mouse model.15
Recent work has identified lysosomes as important mediators of the nonapoptotic PCD induced by type II anti-CD20 mAbs in vitro, with the lysosomal protease cathepsin B, being dispersed into the cytoplasm to trigger cell death.21 If this newly characterized mode of PCD is shown to contribute to the therapeutic efficacy of type II anti-CD20 mAbs in vivo, it has potentially important clinical advantages in B-cell malignancies. First, as this mode of cell death is Fc-independent, it can provide a mechanism of tumor cell kill in patients in which Fc-FcγR–dependent mechanisms are impaired. This can occur, for example, in patients with low-affinity FcγRIIIa, or patients with immune effector cell failure most commonly secondary to chronic depletion by chemotherapy regimens. The latter subset of patients, in particular, may not benefit from mAb design focused entirely on enhancing Fc-FcγR interactions, if their FcγR-expressing cells are deficient or defective. Second, through its ability to bypass the apoptotic machinery, it may help to eradicate tumors that are resistant to apoptosis and that respond poorly to chemotherapy or immunochemotherapy. Such defects in the apoptotic machinery leading to impaired responses to rituximab-containing immunochemotherapy include overexpression of the transcriptional repressor BCL-6 in DLBCL,68 as well as MCL-1 overexpression69 and loss of the tumor suppressor TP53 in B-CLL.11,70,71 Recent studies have shown that the activation of nonapoptotic PCD can eradicate various apoptosis-resistant malignancies, including hormone-refractory prostate cancer72 and glucocorticoid-resistant acute lymphoblastic leukemia.73 In addition, because PCD induced by type II anti-CD20 mAbs appears to be mediated by lysosomal rupture, it will be interesting to examine whether agents that can induce lysosomal destabilization, such as the commonly used cytotoxic drug vincristine,74 will be able to sensitize tumor cells to type II anti-CD20 mAb-induced PCD. The implication in the development of novel anti-CD20 mAbs is that perhaps a greater focus should be made on the ability of mAb to induce direct PCD. The development of rational combination therapies that exploit this novel mode of cell death could also potentially provide hope for clinical responses in patients with rituximab-refractory disease.
Do anti-CD20 mAbs induce a “vaccination” effect?
New data have intriguingly suggested that anti-CD20 mAb may induce an adaptive antitumor immune response or “vaccination” effect, and this may underlie the durable remissions experienced by some patients after anti-CD20 mAb treatment.75 Rituximab-coated lymphoma cell lines have been shown to facilitate the cross-priming of tumor antigens by human dendritic cells and elicit a CD8 T-cell response in vitro.76 A “proof of principle” clinical study demonstrated that rituximab therapy induces an idiotype-specific T-cell response in FL patients.77 More recently, Abès et al showed that an anti-hCD20 mAb induces protection against hCD20-expressing murine lymphoma in an immunocompetent mouse model through a T cell–mediated immune response.78 As more syngeneic, immunocompetent mouse models have become well established over the last decade, it is hoped that they will offer more insight into the importance of this mechanism and how it can be harnessed for anti-CD20 mAb therapy.
What is our current understanding of the mechanisms of rituximab resistance?
An enhanced understanding of the mechanisms of rituximab resistance is central to developing therapeutic strategies and informing the development of novel anti-CD20 mAbs to improve clinical outcomes. Several mechanisms of resistance have been postulated, including increased mAb metabolism, reduced tumor penetration, impaired mAb binding, loss/down-regulation of CD20, resistance of tumor cells to mAb-effector mechanisms, and impaired immune effector cell recruitment or function.79 The contribution of these mechanisms to the clinical resistance to rituximab remains unclear. Several groups have attempted to model rituximab resistance with repeated exposure of lymphoma cell lines to rituximab in vitro. This approach has resulted in cells with reduced CD20 expression, increased resistance to CDC and ADCC,80 and hyperactivated cell survival pathways (NF-κB and extracellular signal–regulated kinase).81 The clinical relevance of these rituximab-resistant cell lines, however, remains undetermined. Emerging clinical evidence supports the contribution of CD20 loss to rituximab resistance, with antigen loss observed in a proportion of patients who have relapsed after rituximab.82 These data challenge the view that CD20 is a stable target that does not shed/internalize on mAb ligation. The Taylor laboratory observed that after B-cell depletion by rituximab infusion in CLL patients, a population of B cells with significantly reduced CD20 levels reemerges in the circulation.45 They demonstrated that this occurs because of “shaving” of rituximab/CD20 complexes by phagocytic cells on saturation of immune effector mechanisms because of high burden of circulating mAb targets.83 Recently, Beers et al84 demonstrated an additional mechanism of rituximab-induced CD20 loss, which occurred through internalization of CD20 and its trafficking to lysosomes in normal B cells and a large panel of primary B-cell malignancies, albeit with marked heterogeneity between individual samples. Studies are ongoing to determine whether the degree of internalization correlates with clinical resistance to rituximab. This recently characterized internalization, unlike shaving, does not require phagocytes. Importantly, the type II anti-CD20 mAb tositumomab, induced significantly less antigenic internalization contributing to its enhanced ability to deplete B cells in hCD20 mice.84 Other investigators have implicated a role for epigenetic mechanisms in down-regulating CD20 expression after rituximab treatment, as CD20 expression in CD20-negative lymphoma cells obtained from a patient who relapsed after R-CHOP was restored by a DNA methyltransferase inhibitor,82 and histone deacetylase inhibitors increased CD20 expression and therapeutic efficacy of rituximab in xenograft models.85 However, the mechanisms of resistance in CD20-positive tumors are yet to be determined and may lie in the failure of immune effector cell recruitment and/or function. This hypothesis requires further clinical investigation.
Next-generation anti-CD20 mAbs
Against this backdrop, it is of interest to evaluate how the new contenders for the throne fare against the incumbent champion rituximab. In particular, whether any of these new anti-CD20 mAbs uses any of the novel mechanistic insights to enhance therapeutic function and lead to activity in rituximab-refractory patients and/or enhanced activity over rituxumab in treatment-naive patients. Currently, there are several new-generation anti-CD20 mAbs, engineered to provide theoretical advantages over rituximab that are currently undergoing clinical investigation (Table 1). The first difference to note of the next generation of mAbs is that they are humanized mAbs, unlike the chimeric rituximab. Some of the newer anti-CD20 mAbs have been designed to deliver improved effector functions, including enhanced FcγR binding, CDC, and PCD (GA101, ofatumumab, PRO13192, AME133V; Table 1). The clinical testing of these mAbs probably provides us with further insights as to which effector mechanism should be harnessed to improve the outcome of patients, particularly patients with rituximab-resistant B-cell malignancies.
Of these novel agents, ofatumumab is at the most advanced stage of clinical development. Ofatumumab is a fully human type I mAb that binds a unique epitope on CD20, resulting in a slow off-rate and an unusually high ability to activate complement. Ofatumumab induced CDC in B-non-Hodgkin lymphoma (B-NHL) lines expressing high levels of complement defense proteins and low levels of CD20 antigen, which fail to undergo CDC with rituximab,86,87 and has been shown to deplete rituximab-resistant CLL cells from whole blood ex vivo.86 Importantly, phase 1/2 studies of ofatumumab in lymphoma and CLL showed a similar toxicity profile to that of rituximab, suggesting that the increased ability of ofatumumab to activate complement does not further increase toxicity.88,89 Ofatumumab showed good activity in relapsed/refractory FL in a phase 1/2 dose escalation study with an overall response rate (ORR) of 43%.89 Encouraged by these results and responses seen in rituximab-refractory patients, a study examining efficacy in 116 patients with FL refractory to rituximab alone or in combination with chemotherapy was conducted. The results of this study, however, were disappointing with an ORR of 11% in this heavily pretreated patient population.90 These findings strongly suggest that ofatumumab monotherapy has little activity in rituximab-refractory FL and also suggest that enhancing CDC may not result in overcoming resistance to rituximab. The possibility still remains that ofatumumab in combination with chemotherapy may enhance tumor responses, and this is being investigated in ongoing trials in both FL and DLBCL.91 The results with ofatumumab in CLL appear more promising in refractory patients. A pivotal, multicenter study conducted by Wierda et al92 has shown that ofatumumab induced substantial numbers of responses in patients refractory to both fludarabine and alemtuzumab (n = 59, 58% ORR) and patients refractory to fludarabine with bulky (> 5 cm) lymphadenopathy (n = 79, 47%). Although impressive response rates were observed, it is important to bear in mind that much higher doses of mAb were administered in this study than have been previously used with rituxumab, with 8 weekly infusions followed by 4 monthly infusions of 2000-mg doses (except the first dose of 300 mg).92 On the basis of these data, ofatumumab has received FDA approval for use in fludarabine and alemtuzumab-refractory CLL, yet its clinical superiority over rituximab or activity in rituximab-refractory CLL patients has not been determined.
Ocrelizumab is a humanized type I anti-CD20 mAb that differs from rituximab at several positions within the complementarity-determining region. Compared with rituximab in vitro, ocrelizumab demonstrated superior binding to the low-affinity variants of the FcγIIIa, increased ADCC, and lower CDC.93 Normal B-cell depletion in nonhuman primates was comparable with that achieved in similar studies with rituximab.94,109 A phase 1/2 trial of ocrelizumab in relapsed/refractory FL resulted in an ORR of 36% (complete response/complete response unconfirmed = 13%), with apparently milder adverse events compared with rituximab.93 Veltuzumab is a humanized type I anti-CD20 mAb with an identical complementarity-determining region to rituximab, apart from one amino acid substitution, resulting in a reduced off-rate. Veltuzumab had similar in vitro activity to rituximab but superior efficacy in lymphoma xenograft models.95 In its first phase 1/2 trial of 82 patients with relapsed/recurrent B-NHL, the ORR (41%) and toxicity profile were comparable with that of rituximab in a similar patient population, but interestingly, veltuzumab was active at 80 mg/m2, approximately 20% of the standard 375-mg/m2 rituximab dose.96 Thus, the investigators initiated a trial of low doses of veltuzumab administered subcutaneously in B-cell malignancies and demonstrated that the mAb achieves slow but efficient delivery into the blood and is pharmacologically active.97
In contrast to the other anti-CD20 mAb in development, GA101 is the first humanized, type II anti-CD20 mAb to enter the clinic. GA101 has a glycoengineered Fc fragment with nonfucosylated oligosaccharides to enhance the interaction with FcγR, particularly FcγRIIIa, therefore enhancing ADCC.110 GA101 demonstrates properties consistent with a bone fide type II anti-CD20 mAb, potently evoking the previously described nonapoptotic PCD and lacking the ability to translocate CD20 into membrane lipid rafts or activate complement.100,101 GA101 has demonstrated superior tumor growth inhibition compared with rituximab in subcutaneous lymphoma xenograft models as monotherapy,101 or in combination with cyclophosphamide in an FL xenograft model,102 and greater B-cell depletion than rituximab in nonhuman primates101 and hCD20 transgenic mice.100
The first phase 1 dose-escalation trials of GA101 were performed in patients with relapsed/refractory B-cell malignancies and B-NHL who were previously exposed to rituximab. ORR values of 58% (7 of 12 patients) and 43% (9 of 21 patients) were seen, respectively, and responses occurred across all FcγRIIIa polymorphisms.103,104 A further phase 1 study of GA101 therapy followed by maintenance was conducted in patients with relapsed/refractory B-cell malignancies, half of whom were refractory to rituximab. Although the ORR was low at 25% in this heavily pretreated population, clinical responses were observed in rituximab-refractory patients.105 In a recent phase 2 study of 2 dose groups of GA101 in relapsed/refractory indolent lymphoma, GA101 was administered weekly for 3 doses, then monthly for a total of 9 infusions at a low (400 mg) and high (1600 mg for the first 2 doses, and 800 mg thereafter) dose. Interestingly, 7 of 24 patients with rituximab-refractory disease responded, 6 of whom received the higher dose.106 In a phase 1 study of relapsed/refractory B-CLL patients, GA101 induced an ORR of 63% (8 of 13) and rapid B-cell depletion107 in a group of patients who would be expected to respond poorly to rituximab monotherapy.111 Currently, studies of GA101 versus rituximab as monotherapy or in combination with chemotherapy are ongoing.103 Any potential improvements observed with GA101 over rituximab in the clinic will be difficult to dissect as being secondary to the type II properties or the glycoengineered Fc. It is however interesting to note that a nonglycoengineered version of GA101 showed superior therapeutic efficacy compared with rituximab in preclinical mouse models.100,108
In addition to the glycoengineered GA101, several novel type I anti-CD20 mAbs have been developed with Fc arms engineered to enhance FcγRIIIa binding and ADCC ability, including AME-133v and PRO131921 (a modified version of ocrelizumab), and are now undergoing early phase 1/2 trials in relapsed B-NHL.98,99 Currently, it appears that the Fc optimization in the next-generation anti-CD20 mAbs is entirely focused on enhancing FcγRIIIa binding. However, given the recent preclinical and clinical data implying a potentially pivotal role for macrophages in anti-CD20 mAb therapy,26,39,84 it is important to consider alternative Fc engineering techniques that target the macrophage interaction, such as that developed by Richards et al in which a novel amino-acid substitution (G236A) provides selectively enhanced binding to FcγRIIa relative to the inhibitory FcγRIIb and thus improves antibody-dependent macrophage phagocytosis.112 Finally, a further understanding of the mechanism underlying innate and acquired rituximab resistance is required to determine whether the enhanced recruitment of immune effector cells by the next-generation anti-CD20 mAb can overcome rituximab resistance or whether this resistance is a manifestation of immune effector function failure, in which case such enhancements may not be effective.
Although many novel anti-CD20 mAbs have been developed, the efficacy of these next-generation mAbs in rituximab-refractory disease or their activity compared with rituximab in responsive disease is yet to be determined. Randomized clinical trials are required to address these questions, some of which are currently ongoing. One confounding factor in the emerging trials is the increased dose of anti-CD20 mAb used in comparison with the standard 375-mg/m2 rituximab dose, making comparison of therapeutic efficacy more difficult.
In conclusion, over the last 10 years, rituximab has revolutionized the treatment of all common B-cell malignancies. This success has catalyzed the development of the next generation of anti-CD20 mAbs, designed to further improve clinical outcomes. The lack of clarity regarding the precise mechanism of action of anti-CD20 mAb in patients is reflected in the variety of approaches taken to improve these novel anti-CD20 mAbs. As these mAbs are tested and compared in the clinic, they will hopefully provide more insights into the mechanisms required to further improve anti-CD20 mAb therapy beyond rituximab. After inspection of the enlarging tool kit of anti-CD20 mAb, it seems that the majority are type I anti-CD20 mAb and appear to be very similar tools to rituximab. Some are designed to have enhanced Fc-dependent functions, such as CDC and FcγR binding. However, if it proves true that enhancing CDC does not improve anti-CD20 mAb efficacy and rituximab resistance is largely dictated by failure of immune effector cell function, then it would seem unlikely that these novel mAbs will result in substantial improvements over rituximab. In this scenario, then perhaps exploiting type II anti-CD20 mAbs, with their ability to directly induce nonapoptotic PCD and limit CD20 modulation, may serve as the “hammer-blow” for rituximab-refractory disease, but this ultimately will need to be determined by rigorous clinic testing. Such clinical testing is currently the only way of establishing the worth of any new anti-CD20 mAb.
As we move into an era of personalized medicine, it will become increasingly important for us to develop closer links between the laboratory and the clinic. For B-cell malignances, this is likely to include tumor profiling, analysis of the microenvironment, such as macrophage profiling, as well as an assessment of host immune effector function and genetic polymorphisms of FcγR. Finally, it will be critical that new insights gleaned from clinical testing are taken back to the laboratory to further refine and enhance the potency of anti-CD20 mAbs.
Acknowledgment
The authors thank Dr Jamie Honeychurch for providing the figure illustration and constructive comments on the manuscript.
Authorship
Contribution: W.A. and T.M.I. wrote the manuscript.
Conflict-of-interest disclosure: T.M.I. has received honorarium for consultancy work with Hoffman La Roche and GlaxoSmithKline. W.A. declares no competing financial interests.
Correspondence: Tim M. Illidge, School of Cancer and Enabling Sciences, School of Medicine, University of Manchester, Manchester, M20 4BX, United Kingdom; e-mail: tmi@manchester.ac.uk.