In this issue of Blood, Zhang et al identify the Src-PLD1-PKCγ axis as critically involved in the process that causes ROP, highlighting new potential targets for therapy.1
Vascular endothelial growth factor (VEGF) is acknowledged as the predominant regulator of angiogenesis; blockade of VEGF signaling is central in therapy for numerous cancers and the vascular retinopathies of diabetes, age-related macular degeneration, and retinopathy of prematurity (ROP). Although anti-VEGF monotherapy shows substantial results, in many cases it is becoming increasingly appreciated that combination therapy will be necessary.2 Tumors have demonstrated various degrees of intrinsic refractoriness or the development of treatment-related resistance. For age-related macular degeneration, expected to soon affect nearly 3 million people in the United States, the optimal therapy of long-term monthly intraocular injections of anti-VEGF agents will likely prove unsustainable for practical and clinical reasons. Thus, effective treatment will require the combination of anti-VEGF therapy with conventional chemotherapeutic agents, radio-therapy or phototherapy, or the targeting of multiple components of VEGF-activated processes.
The breadth of disease states in which VEGF-induced angiogenesis plays a central role correlates to a large and incompletely defined population of regulatory molecules of VEGF signaling, many likely to be tumor/context-specific. The Zhang paper defines the players in a model of ROP and thus identifies potential new specific targets for therapy. In their report, Zhang and colleagues demonstrate that an intact VEGF-signaling axis—constituted by the sequential activation of Src, phospholipase 1 (PLD1), and protein kinase Cγ (PKCγ)—mediates the pathologic neovascularization seen in the oxygen-induced retinopathy model of ROP. This axis was delineated in vitro using chemical inhibitors (1-butanol and propranolol) and in vivo using intraocular administration of siRNAs specific to individual components of the pathway.
Previous work has identified the protein tyrosine kinase activity of Src as a regulator of both VEGF expression and of responses to VEGF stimulation.3 Zhang et al are the first to report activation of PLD1 by Src. Furthermore, they demonstrate that Src-dependent PLD1 activation is required for subsequent activation of PLCγ. The recent development of selective small molecule inhibitors that target Src and the demonstration that Src inhibition can attenuate chemoresistance of some solid tumors suggests a possible clinical use of Src inhibition in vascular retinopathy.
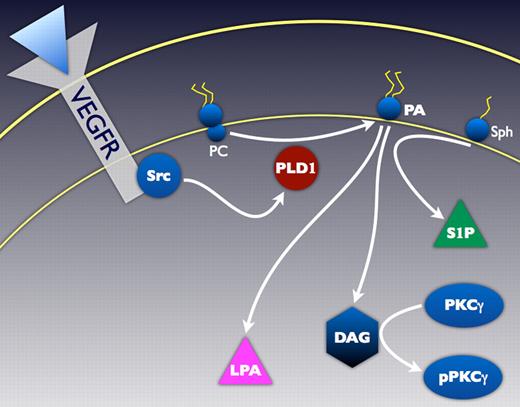
Investigation of the role of bioactive lipids in regulation of angiogenesis is a burgeoning area of research likely to result in a new class of therapeutic agents.4-6 Of particular topical interest are the bioactive lipids PLD1, phosphatidic acid (PA), lysophosphatidic acid (LPA), and sphingosine-1-phosphate (S1P). After activation by any of a variety of intracellular factors (including PKC, Rho, Rac, and certain phosphoinositides) PLD1 hydrolyzes phosphatidylcholine, resulting in the production of PA. PA is considered to be the essential mediator of many of the downstream effects of PLDs. PA can be converted to LPA (implicated in cancer cell and endothelial cell migration and angiogenesis) or diacylglycerol (DAG; crucial in activation of PKCs), and binds to sphingosine kinase, thus assisting in generation of S1P (see figure). S1P has potent effects on vascular inflammation and development and on several endothelial cell functions, including regulation of angiogenesis. In an elegant study, Zeng and colleagues recently demonstrated that PLD1 is required for angiogenesis of intersegmental blood vessels in zebrafish.7 The current study greatly advances our understanding by showing relevance in a mammalian model of pathologic angiogenesis and demonstrating that intraocular administration of PLD1 inhibitors (in this case, siRNA) is an effective technique. Potent pharmacologic inhibitors of PLD have recently been designed and shown effective in blocking PA production.7 As PA plays a central role in the signaling network of VEGF-induced angiogenesis, PLD inhibitors may well have clinical use.
PLD1 mediates production of PA, a central bioactive lipid essential in regulation of VEGF-induced angiogenesis. Details of the pathway and definitions of most abbreviations are in the commentary text. VEGFR indicates VEGF receptor; PC, phosphatidylcholine; and Sph, sphingosine.
PLD1 mediates production of PA, a central bioactive lipid essential in regulation of VEGF-induced angiogenesis. Details of the pathway and definitions of most abbreviations are in the commentary text. VEGFR indicates VEGF receptor; PC, phosphatidylcholine; and Sph, sphingosine.
The integral contribution of members of the PKC family to VEGF-induced angiogenesis is evidenced by clinical trials using PKC inhibitors to treat diabetic retinopathy.4 Of note, most studies have identified PKCα and PKCβII as the active isoforms in this vasculopathy. In fact, activity of the PKCγ isoform is largely considered as limited to neural tissues. By confirming both the expression of PKCγ in endothelial cells and the antiangiogenic effect of inhibition of endothelial PKCγ, Zhang et al provide significant new mechanistic information. Peptide inhibitors of PKCγ are currently under patent for treatment of alcohol withdrawal, suggesting that these inhibitors are effective as well as appropriate for consideration of administration to humans. The limited expression of PKCγ by endothelial cells (induced only in particular pathologic contexts?) implies that there would be few adverse vascular repercussions of inhibition. For treatment of vascular retinopathy, potential neural side effects of PKCγ inhibition might be prevented by local (intraocular) administration.
The limitations of Zhang et al's report readily lead to future directions of study. As partial support in identification of the components of the VEGF-Src-PLD1-PKCγ axis, they used 1-butanol as a specific inhibitor of PLD-mediated production of PA, and propranolol as a specific inhibitor of PA phosphohydrolase (the enzyme that converts PA to DAG). At the doses used in this study, propranolol may also inhibit PKC,8 leading to inhibition of PKC-dependent PLD activation and VEGF expression. Thus, interpretation of some of their in vitro results may be somewhat complicated. In particular, it would leave open potentially larger roles for LPA and S1P in this model of neovascularization. In addition, it is becoming increasingly clear that 1-butanol has “off-target” effects,9 beyond effects on PLD activity. Although results found with “specific” in vivo inhibition of PLD1 and PKCγ (by siRNA technology) consistent with their interpretation of in vitro experiments significantly attenuates these concerns, the use of recently designed isoform-specific PLD and PKC inhibitors would add value.
The experimental model of neovascularization used in this study was designed specifically to mimic the mechanism that results in ROP. It will be of great interest to determine whether the importance of the Src-PLD1-PKCγ axis extends to other forms of pathologic angiogenesis. For example, angiotensin II, the main effector of the renin-angiotensin-aldosterone system, and a therapeutic target in cardiovascular diseases such as hypertension and heart failure, can induce DAG- and PKC-mediated neovascularization in experimental models.10 This study provides significant support for the importance of bioactive lipids in angiogenesis and for the continued assessment of specific PLD inhibitors.
Conflict-of-interest disclosure: The authors declare no competing financial interests. ■