Abstract
Abstract 2748
Prediction of treatment outcome in the context of specific therapies is a major goal of clinical research. Monosomal karyotype has been established as an independent prognostic marker in patients with AML treated with chemotherapy. Our goal was to investigate the prognostic value of a monosomal karyotype (MK) in patients with acute myeloid leukemia (AML) treated with allogeneic hematopoietic cell transplantation (HCT).
We performed a retrospective cohort analysis in patients with high risk AML who received a first allogeneic HCT from an HLA-compatible donor in one out of six major German transplant centers between 01/2005 and 12/2008. Chromosomal aberrations were classified according to ELN criteria. Monosomal karyotype was defined as two or more distinct autosomal monosomies or one single autosomal monosomy in the presence of structural abnormalities. Survival endpoints were analysed in a complete case analysis with Cox regression modelling. Age, Karnofsky performance status, HCT comorbidity index, remission status at HCT, donor type, sex and CMV match were selected as potential confounders a priori for the model while stepwise backward selection was applied to a set of additional covariates including karyotype information. Model selection was based on the likelihood ratio test. We checked the proportional hazard assumption by generating a time-dependent covariate and testing the interaction term with the predictors of the model.
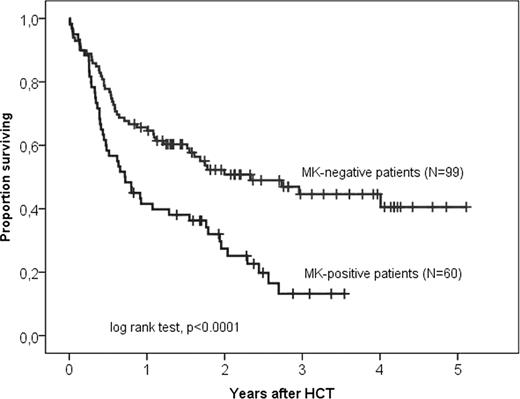
Data from 236 patients with complete karyotype information were analysed. The median age at HCT was 55 years (range, 21 to 77 years). The HCT-comorbidity index was low, intermediate and high in 22%, 27% and 49% of patients. According to ELN criteria chromosomal aberration were classified as intermediate risk in 33% and as high risk in 67% of the patients. The karyotype of 26% of patients met the criteria for a monosomal karyotype. At HCT 60% of patients had less than 5% marrow blasts, 18% had 5 to 20% marrow blasts and 21% had more than 20% marrow blasts. The median interval from diagnosis to HCT was 107 days. Donors were matched siblings in 27%, matched unrelated donors in 49% and partially matched unrelated donors with one to two mismatches in 25% of the patients. Only 16% of the patients were treated with myeloablative conditioning regimens while the remaining patients received reduced intensity conditioning. At the time of analysis, 110 patients were alive with a median follow up of 28 months (range, 8 months to 61 months). Overall survival at 3 years was 51% (95% CI, 42% to 60%) for MK-negative patients and 16% (95% CI, 5% to 27%) for MK-positive patients (log rank test, p<0.0001) (see overall survival by MK-karyotype in high risk patients only in Figure 1). Cox regression modelling was performed as a complete case analysis with data from 221 patients. The cytogenetic classification according to ELN (HR 1.8, p=0.014) and MK karyotype (HR 2.1, p=0.001) together improved the predictive power of the Cox regression model. When MK karyotype was removed from the final model including cytogenetic risk according to ELN the model significantly lost predictive power (likelihood ratio test, p=0.001).
The presence of a monosomal karyotyp is an independent prognostic factor in patients being treated with allogeneic stem cell transplantation and predicts for inferior survival.
Overall survival by MK karyotype in patients with high risk cytogenetic aberrations according to ELN criteria
Overall survival by MK karyotype in patients with high risk cytogenetic aberrations according to ELN criteria
Bug:Celgene: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.