Abstract
Abstract 254
Clinical experience and research with sickle cell patients and those with other genetic diseases suggests that the period of “transition,” in which patients move from pediatric care to adult-centered clinical care, is a period of high health services utilization. Young adult patients may not have learned to effectively manage disease symptoms and may not be connected to a “medical home” or have established a relationship with a primary care physician or adult hematologist. Further, these patients may not have insurance coverage previously provided by parents or by public pediatric insurance programs.
As part of a collaborative agreement through the Centers for Disease Control and Prevention (CDC) and the National Heart, Lung & Blood Institute (NHLBI), California and five other states are conducting epidemiologic surveillance to determine the prevalence of hemoglobinopathies as well as health services utilization. Such data are essential to inform allocation of resources to meet the medical and social service needs of patients. Within the state, this project is a collaborative effort among the CA Dept. of Public Health Genetic Disease Screening Program, Children's Hospital Los Angeles and Children's Hospital & Research Center Oakland. Using administrative data obtained as a part of this effort, we describe emergency room (ER) utilization patterns among young adults with sickle cell disease.
The CA Office of Statewide Health Planning and Development has collected data on ER utilization for the years 2005 – 2008. Using ICD 9 codes beginning with 282.6 to identify sickle cell-related ER visits during those years, we report usage patterns by patient age, gender, and payer type. To calculate risk of repeat ER visits, we used a negative binomial regression model (with 1 visit as the baseline for analysis, rather than 0 visits, due to the limitations of the data set). The following means and counts are adjusted to account for this shift. Analyses were conducted using SAS 9.1.
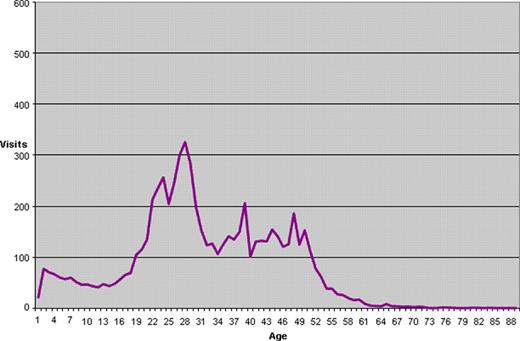
The mean number of ER visits among sickle cell patients in the data set was 3.36 per year and 54% of visits were made by women, but gender differences in average visits per year per patient (3.18 female, 3.60 male) were not statistically significant. Medi-Cal (Medicaid) was the primary payer for 47% of visits during this time frame, and patients with Medi-Cal averaged nearly one additional visit per year (3.82 visits) compared to patients with other forms of payment (3.04 visits). Among patients seen at any time during the four years and controlling for gender and payer type, we found a 78% increase (IRR 1.78, 95% CI 1.59, 2.00) in risk of visiting the ER a second or subsequent time in a given year among the 20 to 30 year old group compared to all other age groups, a four fold increase (IRR 4.22, 95% CI 3.61, 4.93) in risk of a second or subsequent visit in a year compared to the group aged 10 to 20 years, and a 30% increase (IRR 1.34, 95% CI 1.16, 1.55) compared to the group 30 to 40 years of age. Average number of visits in the transition age group was 4.53 per year, compared to 1.93 per year in the 10 to 20y group and 3.56 in the 30 to 40y age group. The number of individuals visiting the ER per year was higher in this age group compared to the two adjoining age groups (520 individuals on average per year for 20 – 30y, vs. 311 per year for 10 – 20y and 355 for 30 to 40y). The increase in visits per year of age can be seen (Figure 1) to begin at age 18 or 19 and continue to approximately age 30. The proportion of patients with no insurance coverage increased from 8% in the 10 to 20y age category to 19% of patients in the 20 to 30y age category, and remains high for the subsequent age categories (11 to 17%).
Mean Annual Number of Visits by Age of Patient among Those Seen in ER with SCD-related ICD 9 Codes, California, 2005–2008
Mean Annual Number of Visits by Age of Patient among Those Seen in ER with SCD-related ICD 9 Codes, California, 2005–2008
Coates:Novartis: Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.