Abstract
Abstract 659
An allogeneic stem cell transplant (SCT) remains the only curative option for patients with β thalassemia major (TM). Conventional risk stratification requires a liver biopsy to be done prior to transplant, has inadequate chelation therapy as a risk factor, which is poorly defined with currently available therapies and results in a large heterogeneous high risk group. We have previously shown that survival can be significantly different in subsets within this high risk group (BBMT 2007;13:889)
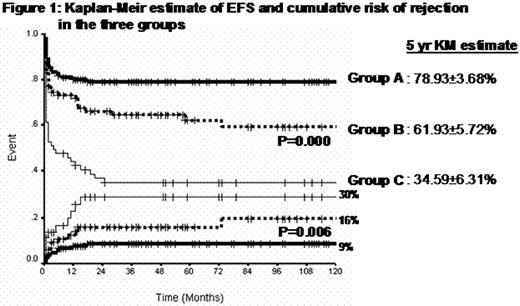
From October 1991 to December 2008, 271 patients with TM underwent a SCT at our center. The median age was 7 years (range: 2-24) and there were 175 males (64.6%). 133 (49%) were conventional Class III patients. Myelo-ablative conditioning regimen in the majority was busulphan (oral) and cyclophosphamide with or without anti lymphocyte globulin. GVHD prophylaxis was cylcosporine and short course methotrexate. Two hundred and sixty six (98%) received a bone marrow graft. At a median follow up of 41 months (range: 0-209) the 5-year Kaplan-Meir estimate of overall survival (OS) and event free survival (EFS) was 70.79±2.9% and 63.75±3% respectively. On a univariate analysis, factors associated with an adverse impact on EFS were patients' age, donor age, liver size, serum AST level, serum ferritin level, number of packed cell transfusions received, spleen size and splenectomy. On a multivariate analysis only liver size (both 2-5 cm and >5 cm) retained its significant adverse impact. The remaining parameters that were significant on a univariate analysis as a continuous variable were further evaluated after dividing them into quartiles. On a cox-regression analysis of the quartiles only age retained significance in all quartiles while the rest were significant only in the highest quartile. For the latter, the cut offs of the highest quartile was used to dichotomize the cohort into two groups for each parameter and a score given proportional to relative risk (Table 1). The total score could therefore range form 0 to 13 for each patient. On a multivariate analysis none of these generated values, including age in the different quartiles, had an independent significant impact on EFS. They were still retained in the scoring system because of the established biological relevance of these parameters on transplant outcomes. Splenectomy was excluded in view of the small number of cases. Kaplan-Meir estimates of EFS were generated for each of these scores and clustered into groups. Three groups could be recognized; Group A with a score <3.5 (n=125 [46%], Group B 3.5-7.5 (n=87 [32%]) and Group C >7.5 (n=59 [22%]). Figure 1 illustrates the Kaplan-Meir estimates of EFS and cumulative risk of rejection between these groups which were significantly different. There were 133 (49%) patients in this cohort who belonged to the conventional Lucarelli Class III subset. Of these, using the current risk stratification 18(13%) would be in Group A, 58(44%) in Group B and 57(43%) in Group C.
| Variables Score . | 0 . | 1 . | 1.5 . | 2 . | 4 . |
|---|---|---|---|---|---|
| Liver size (cm) | <2 | 2-5 | >5 | ||
| Age (years) | <5 | 5-7 | 7-11 | >11 | |
| Packed cell transfusions (units) | <90 | >90 | |||
| Serum AST (IU/Lt) | <75 | >75 | |||
| Serum Ferritin (ng/ml) | <3500 | >3500 | |||
| Spleen size (cm) | <3.0 | >3.0 |
| Variables Score . | 0 . | 1 . | 1.5 . | 2 . | 4 . |
|---|---|---|---|---|---|
| Liver size (cm) | <2 | 2-5 | >5 | ||
| Age (years) | <5 | 5-7 | 7-11 | >11 | |
| Packed cell transfusions (units) | <90 | >90 | |||
| Serum AST (IU/Lt) | <75 | >75 | |||
| Serum Ferritin (ng/ml) | <3500 | >3500 | |||
| Spleen size (cm) | <3.0 | >3.0 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.