Abstract
Abstract 4452
Glycoprotein IIb/IIIa inhibitors (GPI) improve outcomes in patients following percutaneous coronary intervention (PCI) and troponin positive acute coronary syndrome. However, GPI's can result in severe but transient thrombocytopenia (platelet count <50×109 cells/l). Guidelines on management of this complication are lacking. Minimal data exist on clinical outcomes of this cohort of patients and routine prophylactic use of blood products for these patients is controversial.
We aimed to study the clinical course and outcomes of patients with coronary artery disease who were admitted for coronary revascularisation and developed severe thrombocytopenia in coronary care unit of our tertiary cardiac centre.
We undertook review of 50 consecutive patients who had severe thrombocytopenia. Patients were divided in to two groups, severe thrombocytopenia following GPI usage and severe thrombocytopenia without exposure to GPI (control group). Severe thrombocytopenia in control group was due to co-existent sepsis (4), drugs other than GPI (4), myelodysplasia (4) and unknown aetiology (7). Patients with heparin induced thrombocytopenia, pseudo thrombocytopenia and bypass surgery associated thrombocytopenia and who died within 48 hours were excluded (one in each group). We chose in-hospital mortality, 30-day mortality, repeat coronary intervention and major bleeding as defined by TIMI criteria, as our combined primary endpoint.
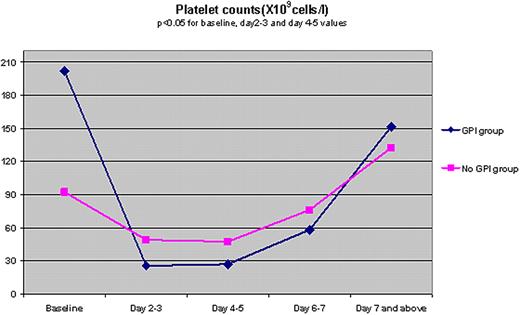
Data from 27 patients with severe thrombocytopenia following GPI administration and 19 age-matched controls were included for analysis. The GPI group had more males (92.6% vs.78.9%), smokers (29.6% vs.3.7%) and patients with a history of hypertension (59.3% vs.57.9%) and dyslipidaemia (66.7% vs.57.9%). Baseline platelet counts were higher in GPI group (in X109 Cells/l, mean, (SD), 201.63 (78.69) vs. 92.2 (8.02), p<0.05). More number of patients in the GPI group had PCI procedures and coronary stents. Patients in GPI group had major fluctuations and quicker recovery of platelet counts (Figure 1). This group had more patients with minor bleeding without any increase in major bleeding (Table 1). GPI group received fewer blood product transfusions (mean units, blood: 0.07 vs.1.32, p<0.05, platelets: 0.22 vs.1.05, p<0.05). GPI group had significant favourable outcomes such as, lower combined primary end point (3.7% vs.42.1%, p<0.05), lower in hospital mortality (3.7% vs.26.3%, p<0.05) and shorter duration of hospital stay (mean days 3.92 vs.25.08, p<0.05) compared to no-GPI group.
GPI related severe thrombocytopenia was not associated with an increase in bleeding complications or adverse cardiovascular events. A conservative approach with minimal blood product replacement was safe in this group of patients. These findings may have implications in minimising blood product support in this cohort of patients.
Time line of platelet counts in patients with and without exposure to Glycoprotein IIb/IIIa inhibitors (GPI).
Time line of platelet counts in patients with and without exposure to Glycoprotein IIb/IIIa inhibitors (GPI).
Outcomes in patients with severe thrombocytopenia. $$Peak to trough ratio= 100X[(highest–lowest platelet count)/highest platelet count]. Value 100 indicates major fluctuation whereas 0 indicates no change. *P <0.05. SD: standard deviation.
| . | GPI group (27) . | No GPI group (19) . |
|---|---|---|
| Had PCI* | 96.3% | 42.1% |
| Number of coronary stents, Mean(SD)* | 2.04 (1.26) | 0.37 (1.16) |
| In hospital death* | 3.7% | 26.3% |
| Combined end point* | 3.7% | 42.1% |
| Major bleeding* | 0 | 15.8% |
| Minor bleeding | 33.3% | 26.3% |
| Blood transfusion, in units, Mean(SD) * | 0.07 (0.38) | 1.32 (1.95) |
| Platelet transfusion, in units, Mean (SD) * | 0.22(0.58) | 1.05 (1.68) |
| Duration of hospital stay. in days, Mean (SD) * | 3.92 (2.62) | 25.08 (30.35) |
| Peak platelet count X109 cells/l, Mean (SD) * | 216.70 (96.62) | 143.37 (86.57) |
| Trough platelet count X109 cells/l, Mean (SD) * | 15.0 (13.47) | 29.37 (9.97) |
| Peak to trough ratio,(SD)*,$$ | 90.54 (12.77) | 71.01 (19.67) |
| . | GPI group (27) . | No GPI group (19) . |
|---|---|---|
| Had PCI* | 96.3% | 42.1% |
| Number of coronary stents, Mean(SD)* | 2.04 (1.26) | 0.37 (1.16) |
| In hospital death* | 3.7% | 26.3% |
| Combined end point* | 3.7% | 42.1% |
| Major bleeding* | 0 | 15.8% |
| Minor bleeding | 33.3% | 26.3% |
| Blood transfusion, in units, Mean(SD) * | 0.07 (0.38) | 1.32 (1.95) |
| Platelet transfusion, in units, Mean (SD) * | 0.22(0.58) | 1.05 (1.68) |
| Duration of hospital stay. in days, Mean (SD) * | 3.92 (2.62) | 25.08 (30.35) |
| Peak platelet count X109 cells/l, Mean (SD) * | 216.70 (96.62) | 143.37 (86.57) |
| Trough platelet count X109 cells/l, Mean (SD) * | 15.0 (13.47) | 29.37 (9.97) |
| Peak to trough ratio,(SD)*,$$ | 90.54 (12.77) | 71.01 (19.67) |
Zaman:British Heart Foundation/FS/07/033: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.