Abstract
Abstract 4340
Although umbilical cord blood (UCB) is an accepted alternative to bone marrow or peripheral blood (BM/PB) for transplantation, allele-matched marrow or peripheral blood is generally regarded as the preferred graft source. Our aim is to compare leukemia-free survival after transplantation of unrelated donor UCB and allele-matched BM/PB, and to provide guidelines for selection of an appropriate donor and graft source in children with acute leukemia.
Outcomes of 22 children with acute leukemia and transplanted with single unit UCB were compared with outcomes of 34 BM/PB recipients. All transplantations were performed in Samsung Medical Center between May 2003 and June 2009. Recipients of UCB were transplanted with grafts that were HLA-matched (n = 3) or HLA-mismatched for one (n = 15) or two antigens (n = 4). BM/PB recipients were transplanted with grafts that were HLA-matched (n = 20) or mismatched (n = 14). While allele-level typing for HLA-A, HLA-B, HLA-DRB1 and antigen-level typing for HLA-C was used for BM/PB transplantation, antigen level typing for HLA-A, HLA-B and HLA-DRB1 was used for UCB transplantation. Myeloablative conditioning regimens were used for both BM/PB and UCB transplantation.
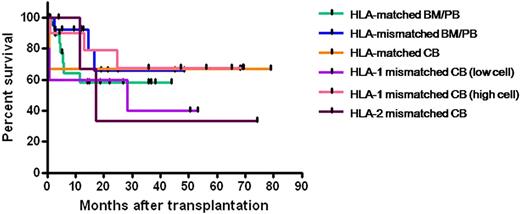
The median times to neutrophil and platelet recovery were 15 (range 10–21) and 22 (12–29) days after BM/PB transplantation, and 17 (13–44) and 34 (24–148) days after UCB transplantation, respectively. The 4-year probabilities of leukemia-free survival were 58.0% after HLA-matched BM/PB transplants, 65.9% after HLA-mismatched BM/PB transplants, 66.7% after HLA-matched UCB transplants, 67.5% after one-mismatched UCB transplants with high cell dose (NC > 3.0 × 107/kg), 40.0% after one-mismatched UCB transplants with low cell dose (NC < 3.0 × 107/kg), and 33.3% after two-mismatched UCB transplants. The incidence of grade 3-4 acute graft-versus-host disease (GVHD) were 12.1% after BM/PB transplantation and 5.3% after UCB transplantation, respectively (P = 0.64). Rates of extensive chronic GVHD were 53.8% after BM/PB transplantation and 23.1% after UCB transplantation, respectively (P = 0.09). Transplant-related mortality rates were higher after UCB transplantation (21.7%) than BM/PB transplantation (2.9%) (P = 0.03). Relapse rates were similar after BM/PB transplantation (29.4%) and UCB transplantation (21.7%) (P = 0.56).
These results support the use of HLA-matched or one-antigen HLA mismatched UCB in children with acute leukemia who need transplantation. Faster identification of a suitable cord blood unit may result in a timely transplantation avoiding delay that could expose the patient to the risk of losing the eligibility for transplant due to relapse or other complications.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.