Abstract
Abstract 3327
Poster Board III-215
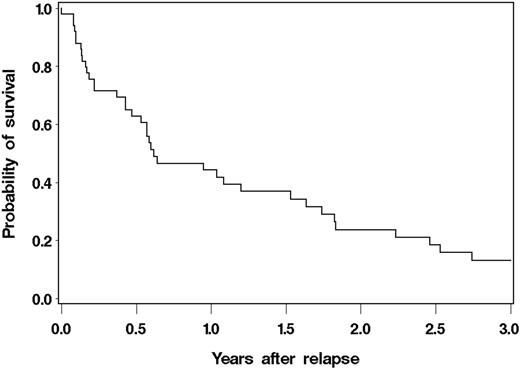
Mantle cell lymphoma (MCL) exhibits short remission durations and a poor prognosis. To improve outcomes, many have advocated the use of high-dose therapy (HDT) and autologous hematopoietic stem cell transplantation (ASCT). However, most data indicate that ASCT is not curative with nearly all patients eventually relapsing. Since little is known regarding the outcomes of these individuals, we retrospectively evaluated MCL patients relapsing after HDT and ASCT and described the association of factors with survival. A total of 134 consecutive MCL patients received HDT and ASCT at our center from 1996 to 2009. Among them, 51 has relapsed so far (38%). Their baseline characteristics included: median age at diagnosis = 57 years (range, 35-70), median age at transplant = 59 years (range, 35 – 70), stage III-IV at diagnosis=98%, median LDH/upper limit of normal (ULN) at diagnosis = 1.14 (range, 0.56 -5.65), median LDH/ULN at transplant = 0.92 (range, 0.58-3.00), median white blood cell (WBC) count at diagnosis = 9.70 × 109 /liter (range, 1.40 – 48.00), mean WBC count at transplant = 5.30 × 109 /liter (range, 0.10 – 17.60), median number of prior chemotherapy regimens = 2 (range, 1-5). The median time to relapse following ASCT was 0.97 years (range: 0.08 – 5.61). Seven patients (14%) received a non-ablative allogeneic transplant (NMAT) for the treatment of relapse after ASCT. Of the 51 patients who relapsed, 40 (78%) have died. Overall survival at 3 years after relapse was 13.2% (95% CI, 4.9-25.5) (Fig.1). The MCL international prognostic index (MIPI) at diagnosis (MIPI-Dx) was a predictor of OS when evaluated either as a categorical variable (0-3 vs. 4 vs. 5-9, p=0.05, global test) or continuous linear variable (p=0.005). When compared to patients with a MIPI-Dx of 0-3, those with a score of 5-9 had a 3.5 (95% CI 1.3-9.7) fold higher risk of mortality after relapse. Similarly the MIPI at autologous transplant (MIPI-Trx) was also a significant predictor of OS after relapse when evaluated as a continuous linear variable (p=0.01). A multivariable model of all factors collected at ASCT identified ECOG performance status (PS)>0 (HR 2.1, 95% CI 1.0-4.2), TBI-based conditioning regimen (HR 4.3, 95% CI 1.8-10.0) and transplant beyond 1st remission (HR 3.5, 95% CI 1.5-8.0) as associated with a significantly higher risk of mortality after relapse; whereas time to relapse from transplant >1 year (HR 0.1, 95% CI 0.04 -0.5) was associated with lower risk of mortality. For example, patients relapsing one year or later after transplant had an estimated 1-year survival after relapse of 76% compared to 17% for those who relapsed earlier (Fig.2); patients transplanted in CR/PR1 had an estimated 1-year survival of 75% after relapse compared to 28% transplanted beyond first remission. These results indicate that OS following relapse of MCL after HDT and ASCT is poor, with the worst outcomes in those with early relapse, transplant later in the disease course, poor PS, TBI-based HDT, and high MIPI score. Only a small minority of patients attempted salvage with NMAT after relapse. These data can be used to better counsel patients and optimize treatment strategies based on the identified mortality risk factors, as improved outcomes are clearly needed in this population.
OS of all MCL patients after relapse
OS of MCL patients who relapsed < 1 year after ASCT and those relapsed ≥ 1 year after ASCT
OS of MCL patients who relapsed < 1 year after ASCT and those relapsed ≥ 1 year after ASCT
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.