Abstract
Abstract 1518
Poster Board I-541
Chronic blood transfusions are commonly used as therapy for sickle cell disease (SCD, HbSS) in order to improve oxygen delivery and minimize complications such as stroke in high-risk children. Vaso-occlusive crises can occur in regions of high shear flow (e.g., major cerebral artery occlusions) or regions of low shear flow (e.g., marrow infarct) leading to acute ischemia and, if severe, to necrosis of affected tissues. Transfusion with normal (AA) RBC causes an increase of hematocrit (H) that is complicated by two opposing factors: increased hematocrit (H) causes a linear increase of oxygen carrying capacity and also an exponential increase of blood viscosity (η). As a consequence, the calculated oxygen transport effectiveness, defined as the ratio of H to η (H/η), is a biphasic function of hematocrit: H/η initially increases with H, reaches a maximum at an optimal H value, and then declines with further increases of H. At equal H and shear rate, sickle (SS) blood has significantly higher viscosity than AA and hence part of the strategy for transfusing SCD patients is to reduce η so as to improve H/η. Viscosity studies at high shear rates indicate that an optimum H can be demonstrated for AA-SS RBC mixtures prepared by adding AA RBC to SS blood to simulate transfusion. In marked contrast, low shear rate results for AA-SS mixtures indicate that there is no optimum hematocrit and H/η always decreases with increasing H (Transfusion 46:912-918, 2006). In order to extend these previous in vitro observations to SCD patients, we have measured blood viscosity and hematocrit using whole blood samples acquired prior to and following routine therapeutic transfusion; H/η was calculated over a wide, physiologically relevant shear rate range.
All subjects (n= 8, mean age =18.7 years) had homozygous HbSS disease, were crisis-free for > 4 weeks, and were enrolled in a chronic transfusion protocol designed to yield < 30% HbS and a post-transfusion H of 30-35%. Blood samples were obtained pre- and within 120 hours post-transfusion. A computer-controller tube viscometer was used to determine blood viscosity (37 °C, 40 mm Hg oxygen tension) over a shear rate range of 1 – 1,000 1/s.
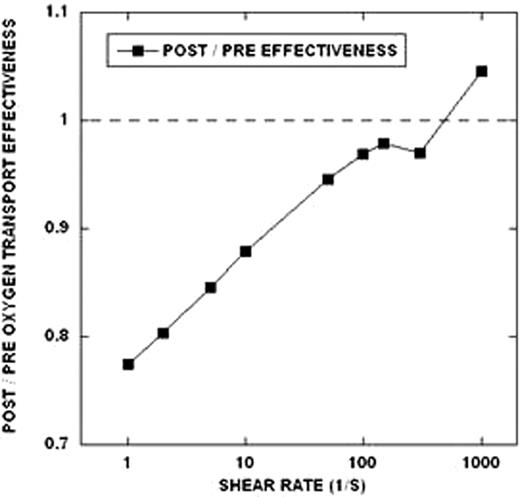
1) As anticipated, blood viscosity and the degree of non-Newtonian flow behavior increased with H (24.7% pre-transfusion, 34.6% post-transfusion); 2) the change of H/η from pre- to post- transfusion was markedly affected by shear rate (Figure). As indicated, there is a large adverse effect at low shear (i.e., H/η reduced by 20-25% following transfusion), a neutral effect at about 50-100 1/s, and an improved H/η at high shear (Figure). That is, transfusion with AA RBC to obtain a lower percent SS RBC and a higher H actually impairs oxygen transport effectiveness at low shear and is only beneficial at high shear.
Clinical experience suggests that transfusion regimens aimed a keeping HbS at 30-50% are effective in preventing recurrent strokes in high-risk children. However, our new in vivo transfusion data suggest that at low shear rates, %HbS must be reduced further for H/η to surpass pre-transfusion levels. We interpret these findings as being consistent with our previous data for AA-SS RBC mixtures. They are also consistent with clinical results indicating lack of efficacy for transfusion in low flow areas (e.g., bone marrow during acute crisis) but highly beneficial effects in high flow regions (e.g., cerebral arteries). Our results thus suggest that benefits of transfusion may vary depending on local flow rates (i.e., shear rates) and organ-specific hemodynamics.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.