Abstract
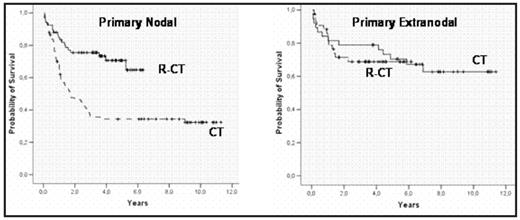
Diffuse large B-cell lymphoma (DLBCL) is a heterogeneous category of lymphoid tumors that comprises different clinical forms not fully recognized in the WHO classification. In this regard, extranodal (EN) DLBCLs have particular clinicobiological features and outcome, sometimes related to the specific site where the lymphoma arises. Nowadays, rituximab plus chemotherapy (CT) is the gold-standard in the treatment of DLBCL. However, the superiority of rituximab-CT (R-CT) over CT alone has not been addressed for all the clinical subsets of the disease and, in fact, the clinical role of the new therapies might be different for primary nodal or EN DLBCLs. The aim of this study was to assess the impact of rituximab in patients suffering from nodal or EN DLBCL. Two-hundred and thirty non-immunocompromised patients (112M/118F; median age, 61 years) diagnosed with CD20+DLBCL in a single institution between 1997 and 2006 (five years before and after establishing R-CT as the standard treatment in DLBCL) and treated with adriamycin-containing regimens were the subject of the present study. The series included 148 primary nodal and 82 EN DLBCL. Patients with primary CNS lymphoma were excluded and lymphomas arising at Waldeyer ring were considered as nodal DLBCL. The main EN sites were GI (n=26), bone (n=13), soft tissue (n=13), lung/pleura (n=9), liver (n=9), and other (n=12). Main clinico-biological and evolutive variables were analyzed. One hundred nineteen patients received only CT and 111 R-CT. Eighty-seven cases with available information were assigned to germinal center B-cell-like (GCB) (41%) or non-GCB (59%) groups according to the Hans method (
| . | Complete response CR (%) . | 5-years OS (%) . | ||
|---|---|---|---|---|
| . | CT . | R-CT . | CT . | R-CT . |
| *p<0.002 R-CT vs. CT | ||||
| All cases (n=230) | 59 | 79* | 46 | 70* |
| Primary nodal (n=148) | 54 | 78* | 34 | 71* |
| Primary extranodal (n=82) | 68 | 78 | 70 | 69 |
| . | Complete response CR (%) . | 5-years OS (%) . | ||
|---|---|---|---|---|
| . | CT . | R-CT . | CT . | R-CT . |
| *p<0.002 R-CT vs. CT | ||||
| All cases (n=230) | 59 | 79* | 46 | 70* |
| Primary nodal (n=148) | 54 | 78* | 34 | 71* |
| Primary extranodal (n=82) | 68 | 78 | 70 | 69 |
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author