Abstract
CNS relapse is a devastating and usually fatal complication of NHL, and controversy exists regarding the best methods of CNS prophylaxis. We have previously shown that IT alone is inadequate in patients (pts) with aggressive NHL at high risk of CNS relapse (
Methods: from 1/91 to 3/08, 85 pts with newly diagnosed aggressive NHL and negative baseline CSF cytology were treated with CNS prophylaxis due to risk factors such as multiple extranodal (EN) sites and elevated LDH. Patients were classified into 3 groups:
CHOP-like therapy & IT (n=24),
systemic therapy incorporating HD-MTX (≥1g/m2 eg Hyper-CVAD; n=25) and
CHOP-like therapy & IT followed by 2 doses of MTX 3g/m2 24 hour CIVI q14d (n=36).
Results: Median age was 52 years (16–82). Groups 1, 2 and 3 were similar in proportions of advanced stage (III and IV), baseline LDH >1× ULN, gender, performance status and number of extranodal sites. Groups 2 & 3, who both received HD-MTX, were similar and were combined for all analyses. The CNS risk index (
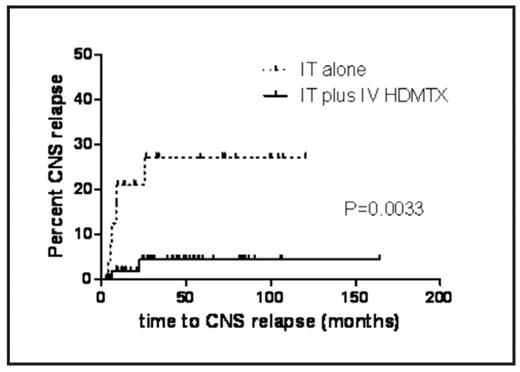
Conclusion: These data demonstrate that IT alone is inadequate CNS prophylaxis in at-risk patients with aggressive NHL. The addition of systemic HD-MTX either as part of primary therapy or administered following CHOP-like therapy significantly reduces CNS recurrence and may improve overall survival.
SEQ Figure \* ARABIC 1: CNS relapse in patients receiving IT chemotherapy alone compared to IT plus IV HD-MTX
SEQ Figure \* ARABIC 1: CNS relapse in patients receiving IT chemotherapy alone compared to IT plus IV HD-MTX
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author