Abstract
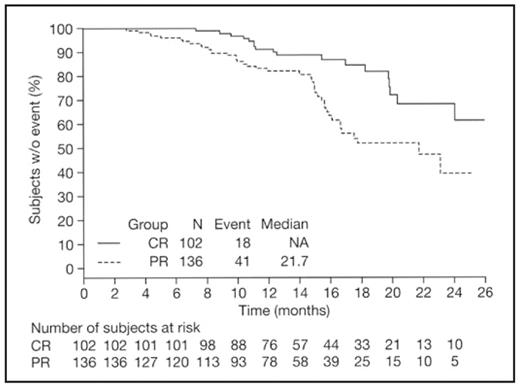
Complete response (CR) has been shown to be prognostic for improved long-term outcomes, including progression-free survival and overall survival (OS), in previously untreated multiple myeloma (MM) patients receiving high-dose therapy and stem cell transplant (SCT; Harousseau et al, IMW 2007; van de Velde et al, Haematologica 2007). However, there is limited evidence of such a correlation in the non-transplant setting. In the large, international phase III VISTA study in previously untreated MM patients ineligible for SCT, bortezomib plus melphalan–prednisone (VMP) demonstrated superiority to MP across all efficacy end points, including response rates, time to progression (TTP), and OS. Here, we assess the differential prognostic impact of best response on time-to-event parameters in VISTA, and evaluate the impact of timing of CR on outcome in patients receiving VMP. A total of 682 patients (median age 71 years) were randomized to receive nine 6-week cycles of VMP (N=344; bortezomib 1.3 mg/m2, days 1, 4, 8, 11, 22, 25, 29, 32, cycles 1–4, and days 1, 8, 22, 29, cycles 5–9, plus melphalan 9 mg/m2 and prednisone 60 mg/m2, days 1–4, cycles 1–9) or MP (N=338). The primary end point was TTP. Response and progression were determined using European Group for Blood and Marrow Transplantation (EBMT) criteria; in a post-hoc analysis, response was determined using International Myeloma Working Group (IMWG) uniform criteria. Associations between long-term outcomes and response were examined in the intent-to-treat population by multivariate Cox regression analysis with time-dependent covariates, adjusted for stratification factors (baseline β2-microglobulin and albumin; region), with age, sex, race, MM type, baseline Karnofsky Performance Status, and number of bone lesions as covariates. Among evaluable patients, response rates to VMP vs MP were 71% vs 35%, including 30% vs 4% CR, by EBMT criteria, and 74% vs 39%, including 33% vs 4% CR and 8% vs 4% VGPR, by IMWG criteria. Median TTP was 24.0 vs 16.6 months. CR by EBMT criteria was associated with significantly longer TTP (hazard ratio [HR] 0.45, p=0.004; Figure), time to next therapy (TNT; HR 0.44, p=0.014), and treatment-free interval (TFI; HR 0.37, p=0.004) vs PR, plus improved OS (medians not reached; clear separation between the curves; HR=0.59, p=0.265; statistical significance not seen likely due to a small number of deaths). Significant benefit was seen for CR and PR vs no response by EBMT criteria for all four parameters, including OS. Findings were similar for CR vs VGPR+PR vs no response by IMWG criteria. Importantly, CR was associated with significantly longer TTP (HR 0.45, p=0.019) and TFI (HR 0.39, p=0.026) vs VGPR, with a trend towards longer TNT (HR 0.54, p=0.126); no significant differences for these parameters were seen for VGPR vs PR. However, these findings should be interpreted with caution due to the small number of patients achieving VGPR. Among patients achieving CR (EBMT criteria) with VMP, there were no clear differences in clinical benefit associated with achieving CR early (cycles 1–4, within 24 weeks) vs later (cycle 5 onwards, after 24 weeks), although TTP and overall duration of response appeared slightly longer with later CRs, possibly due to the inherent slightly longer duration of therapy (mean 7.4 vs 8.5 cycles). In conclusion, this analysis demonstrates the prognostic significance of CR on long-term outcomes in the setting of non-intensive therapy. The data show that CR is associated with improved outcomes vs VGPR by IMWG criteria, and indicate that the clinical benefit of CR with VMP is similar regardless of time to achieve CR, supporting continuation of therapy to achieve maximal response.
Disclosures: Harousseau:Orthobiotech: Honoraria, Speakers Bureau; Janssen Cilag: Honoraria, Speakers Bureau; Pharmion: Honoraria, Speakers Bureau; Celgene: Honoraria, Speakers Bureau. Palumbo:Janssen Cilag: Consultancy, Honoraria. Richardson:Millennium: Honoraria, Membership on an entity’s Board of Directors or advisory committees, Speakers Bureau; Celgene: Honoraria, Membership on an entity’s Board of Directors or advisory committees, Speakers Bureau; Johnson and Johnson: Honoraria, Speakers Bureau. Dimopoulos:Ortho-Biotech: Honoraria. Shpilberg:Johnson & Johnson: Honoraria, Membership on an entity’s Board of Directors or advisory committees. Kropff:Ortho Biotech: Consultancy, Honoraria. Delforge:Janssen-Cilag: Consultancy, Membership on an entity’s Board of Directors or advisory committees. Schots:Celgene: Consultancy, Honoraria; Pharmion: Consultancy. Cavo:Janssen-Cilag: Honoraria, Membership on an entity’s Board of Directors or advisory committees; Millennium: Honoraria, Membership on an entity’s Board of Directors or advisory committees. Golenkov:Johnson & Johnson: Membership on an entity’s Board of Directors or advisory committees, Research Funding. Mateos:Janssen Cilag: Membership on an entity’s Board of Directors or advisory committees. Cakana:Ortho Biotech: Employment. Liu:Johnson & Johnson: Employment, Equity Ownership. Deraedt:Johnson & Johnson: Employment, Equity Ownership. van de Velde:Helgi van de Velde: Employment, Equity Ownership. San Miguel:Ortho Biotech: Membership on an entity’s Board of Directors or advisory committees; Millennium: Membership on an entity’s Board of Directors or advisory committees; Celgene: Membership on an entity’s Board of Directors or advisory committees; Pharmion: Membership on an entity’s Board of Directors or advisory committees.
Author notes
Corresponding author