Abstract
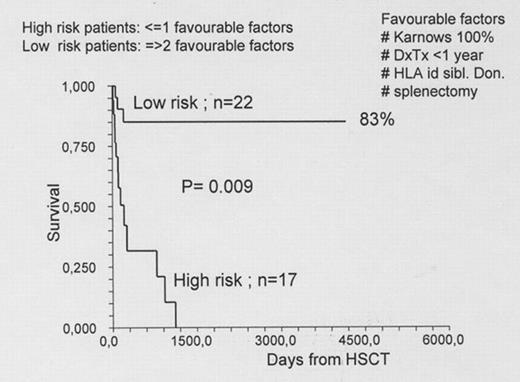
We are reporting the outcome of 39 patients with idiopathic myelofibrosis (IMF) who received an allogeneic hemopoietic stem cell transplant (HSCT) at a single Institution. Patients. The conditioning was a thiotepa - cyclophosphamide based reduced intensity regimen, and graft versus host disease (GvHD) prophylaxis was cyclosporin and methotrexate. 30 patients received marrow, 9 peripheral blood. The donor was an HLA identical sibling (ISD) (n=22) or an alternative related or unrelatd donor (UD) (n=17). The median age was 51 (32–67), the median interval diagnosis HSCT was 1015 days (225–7178) and the Lille risk score at the time of transplant was intermediate in 23 and high in 16 patients. Splenectomy was performed in 25 patients as a preparation for transplant. Results. The overall actuarial survival is 50% with a median follow up of 823 days (221– 4356). In univariate analysis favourable factors for survival were a Karnowsky score of 100% (93% vs 37%), an interval diagnosis transplant of less than 1 year (85% vs 55%), an HLA identical sibling donor (68% vs 47%) and splenectomy pre-transplant (60% vs 50%). When combined together, 17 and 22 patients has 0–1 or 2–3 favourable factors pre-transplant: their 4 year actuarial survival is respectively 0% vs 83% (p=.0001). Patients with 0–1 favourable factors, had higher transplant related mortality (41% vs 0%; p=0.009) and higher relapse related death (35% vs 4%, p=0.01). Conclusions. We conclude that allogeneic transplantation is a curative option for patients with idiopathic myelofibrosis. We have identified factors which predict a favourable outcome and may be used to select patients for this procedure.
Author notes
Disclosure: Consultancy: Pfizer, Roche, Amgen. Research Funding: Pfizer, Roche, Amgen. Honoraria Information: Speakers agreement. Membership Information: Speakers agreement.