Abstract
INTRODUCTION: Non-neoplastic chronic portal vein thrombosis (PVT) has become a more frecuent diagnosis in the course of liver cirrhosis, with reported prevalences of 4,4% to 15,8%. PVT can motivate life-threatening complications due to worsening portal hypertension. The role of anticoagulation in patients with chronic PVT is not well established, and is considered challenging in cirrhotic patients.
OBJECTIVE: To analyze the response to antithrombotic therapy in 12 patients with chronic PVT associated with cirrhosis, and to assess its tolerance and safety.
PATIENTS AND METHODS: 12 consecutive patients with liver cirrhosis and chronic PVT were treated with antithrombotic therapy from 2005 to 2006. PVT was diagnosed by imaging procedures, and was classified as complete or partial according to absence or reduction of blood flow in the portal trunk, branches, superior mesenteric and splenic veins. Hepatocellular carcinoma and known thrombophilic risks were ruled out. Cirrhosis was scored according to Child-Pugh’s classification. History of hemorrhagic episodes was assessed. Therapy was started with 15 days of therapeutic doses of low molecular weight heparin (LMWH) (enoxaparin) adjusted according to baseline hipocoagulability (Table 1), followed by either prophylactic doses (0,5mg/kg/day) of LMWH or acenocoumarol (target INR 2–3), during 6 months. Response was evaluated after 3 and 6 months.
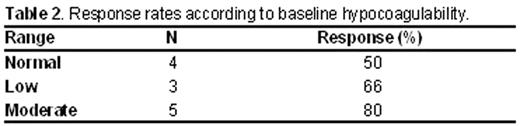
RESULTS: From the 12 patients studied, 9 (75%) were males with a median age of 52 years old (range 35–72). Cirrhosis was due to alcoholism (41%), virus (33%), mixed in one patient and other causes in two patients. Two (16%) patients belonged to Child Pugh’s class A, 6 (50%) to class B and 4 (33%) to class C. Six patients (50%) had previous hemorrhagic episodes due to esophageal varices. PVT involved the portal trunk and/or branches in 91% of the cases, and in 1 patient coexisted with splenic and mesenteric vein thrombosis. Complete thrombosis was seen in 4 patients and partial in 8. From the 12 patients, 8 (66%) responded to antithrombotic therapy after 6 months, with a complete recanalization in 7 patients (87%). Interestingly, the moderate hipocoagulability level subgroup showed an 88% of response (Table2). After an overall follow-up of 6 months, none of the 12 patients presented hemorrhagic complications and none showed platelets counts below baseline values. Acenocoumarol and LMWH were well tolerated in all cases, with only one patient with intolerance to the subcutaneous injections.
CONCLUSIONS: Antithrombotic therapy in chronic PVT in cirrhotic patients showed a high response rate (66%) in our study, with a complete recanalization in 87% of the cases. Adjusted dose scheme according to level of hypocoagulability seems to be effective and safe, since 80% of the subgroup of moderate hypocoagulability responded with no haemorrhagic complications.
Ranges of baseline coagulation study and adjusted therapeutic doses of LMWH. N, Normal range, LH, Low hypocoagulability; MH, Moderate hypocoagulability.

Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author