Abstract
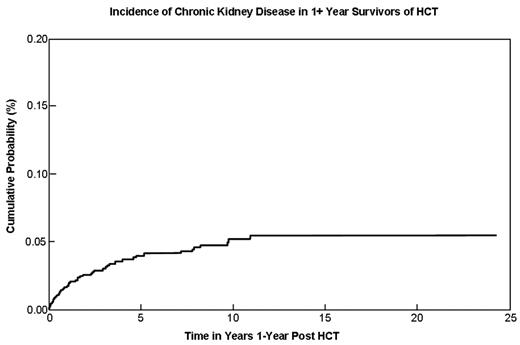
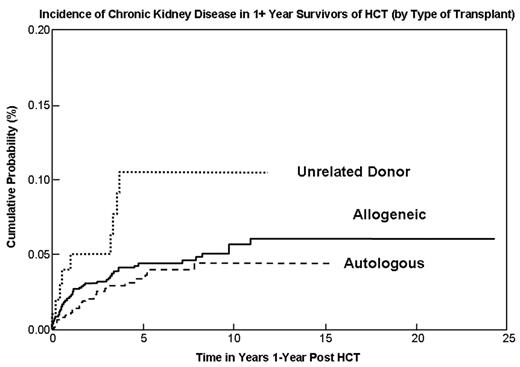
Exposure to pre-transplant nephrotoxic agents, total body irradiation (TBI), and presence of chronic graft-versus-host disease (cGVHD) have been identified as risk factors for developing CKD after HCT. However, small sample size, short follow-up post-HCT, and varying definitions of CKD have precluded a precise estimation of the magnitude of risk and associated risk factors. The aim of the current study was to describe the incidence and risk factors associated with the development of delayed CKD in HCT survivors. Eligible subjects underwent HCT for hematological malignancies or severe aplastic anemia at City of Hope, survived at least one year post-transplant, and were free of CKD at one year post-HCT. Information on pre-transplant therapeutic exposures and post-transplant CKD was obtained via medical record abstraction. All CKD cases were defined according to the National Kidney Foundation’s definition based on glomerular filtration rate (GFR) values. The endogenous filtration marker creatinine was used to estimate GFR values. CKD was defined as a sustained elevation of serum creatinine which infer a GFR of less than 60 mL/min/1.73 m2 for 3 months or longer. The equation used to calculate GFR was as follows: GFR = 186 x (Pcr) −1.154 x (age) − 0.203 (x 0.742 if female) (x 1.210 if African American). Totally, 1,546 eligible subjects were identified (median age at HCT of 34.4, median length of follow-up 6.2 years; autologous HCT in 718 patients [46%], related donor HCT in 726 patients [47%], and unrelated donor HCT in 102 patients [7%]; 59% of subjects (n=913) were male). A total of 65 patients were identified with CKD, resulting in a cumulative incidence of 3.6% [95% confidence interval (CI), 2.6% to 4.6%] at five years post–HCT and 4.8% at 10 years (autologous HCT: 2.9% at five years; matched sibling HCT: 4.1%; matched unrelated donor HCT: 10.5%, p<0.05). In allogeneic transplant recipients, older age at HCT (RR per increase of five years, 1.34; 95% CI, 1.30 to 1.38), prophylaxis/treatment of GvHD with cyclosporine and/or tacrolimus (RR, 4.32; 95% CI, 1.25 to 14.89), and a primary diagnosis of Multiple Myeloma (RR=5.38, 95% CI=1.79 to 16.15) were associated with increased risk. For autologous transplant recipients, older age at HCT was associated with increased risk (RR per increase of five years, 1.33; 95% CI, 1.29 to 1.38). Of note, use of TBI, and chemotherapeutic agents for conditioning, and a history of fungal infection were not associated with risk of delayed CKD development. This study describes the magnitude of risk of delayed chronic kidney disease in a large cohort of long-term survivors of autologous and allogeneic HCT, as well as identifies high risk groups in this population, thus setting the stage for appropriate long-term follow-up of the vulnerable sub–groups.
Incidence of Chronic Kidney Disease in 1+ Year Survivors of HCT
Incidence of Chronic Kidney Disease in 1+ Year Survivors of HCT (by Type of Transplant)
Incidence of Chronic Kidney Disease in 1+ Year Survivors of HCT (by Type of Transplant)
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author