Abstract
We developed a new HCT-specific comorbidity index (HCT-CI) as a sensitive tool to capture pretransplant comorbidities among pts given allogeneic HCT (
Sorror et al. Blood. 2005; 106, 2912–2919
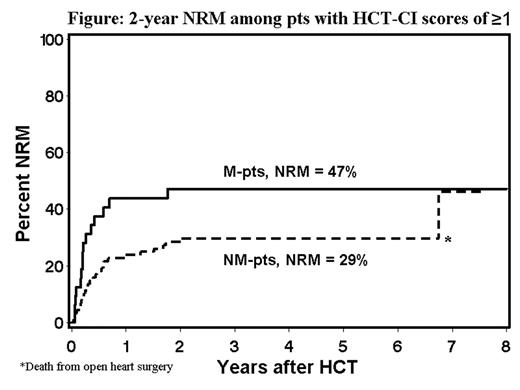
). Here, we retrospectively analyzed whether the HCT-CI was useful in assessing how pts with B cell malignancies tolerated NM vs M-HCT. Results among consecutive pts (n=125) given NM-conditioning with 2Gy total body irradiation (TBI) (19%) or 2 Gy TBI combined with 90 mg/kg of fludarabine (81%) were compared to those among concurrent M-pts (n=55) conditioned with cyclophosphamide plus busulfan (15%) or 12Gy TBI (85%). Diagnoses were non-Hodgkin lymphoma (NHL, 80% vs 52%), Hodgkin disease (HD, 5% vs 20%), and chronic lymphocytic leukemia (CLL, 15% vs 28%), respectively. At HCT, NM-pts differed substantially from M-pts with respect to age (median 52 vs 40 years,), prior treatment regimens (median 5 vs 3), prior failed high-dose HCT (45% vs 9%), unrelated donors (43% vs 18%), and G-PBMC as stem cell source (99% vs 78%). Smaller differences existed for disease chemo-sensitivity (58% vs 69%) and aggressive disease (56% vs 64%). HCT-CI scores >0 were found among 70% and 58% of NM and M-pts, respectively. After HCT, 2-year NRM and survival were 26% and 59% vs 29% and 51% among NM and M-pts, respectively. There were no statistically significant differences in NRM (19% vs 4%, p=0.3) and survival (70% vs 70%, p=0.7) between NM and M-pts with HCT-CI scores of 0; however, this comparison was limited by the small numbers of non-relapse deaths. NM-pts with HCT-CI scores of ≥ 1 had statistically significantly lower NRM (29% vs 47%, HR=0.50, p=0.03, Figure) and better survival (54% vs 37%, HR=0.60 p=0.05) compared to M-pts. These differences remained after adjusting for pretransplant differences (NRM, HR=0.3, p=0.006; survival, HR=0.33, p=0.002). In a further analysis which included all pts, increasing HCT-CI scores and M-conditioning were important risk factors for NRM and survival (Table). We concluded that pts with B cell malignancies and HCT-CI scores of ≥1 tolerated NM-HCT better than M-HCT, and prospective randomized trials may be warranted to confirm this result. Additional data are needed to clarify possible differences between M and NM-conditioning for patients without comorbidities.Table:
Multivariate risk factors for HCT outcomes
| . | . | NRM . | Survival . | ||
|---|---|---|---|---|---|
| . | . | HR . | p . | HR . | p . |
| *Lower HR means better survival. Other risk factors, including donor type; CMV sero-status; and disease chemo-sensitivity, were not significant. | |||||
| Conditioning | NM | 1.0 | 1.0 | ||
| M | 3.03 | 0.007 | 2.27 | 0.006 | |
| HCT-CI scores | 0 | 1.0 | 1.0 | ||
| 1–2 | 2.56 | 1.78 | |||
| ≥3 | 3.85 | 0.001 | 2.44 | 0.005 | |
| Diagnoses | NHL | 1.0 | 1.0 | ||
| HD | 0.79 | 0.98 | |||
| CLL | 0.55 | 0.3 | 0.46 | 0.03 | |
| Graft | G-PBMC | 1.0 | 1.0 | ||
| Marrow | 0.23 | 0.03 | 0.38 | 0.03 | |
| Age, years | <50 | 1.0 | 1.0 | ||
| ≥50 | 2.72 | 0.01 | 1.53 | 0.14 | |
| Prior regimens | 1–2 | 1.0 | 1.0 | ||
| 3–5 | 2.02 | 1.71 | |||
| ≥6 | 0.79 | 0.02 | 1.44 | 0.24 | |
| . | . | NRM . | Survival . | ||
|---|---|---|---|---|---|
| . | . | HR . | p . | HR . | p . |
| *Lower HR means better survival. Other risk factors, including donor type; CMV sero-status; and disease chemo-sensitivity, were not significant. | |||||
| Conditioning | NM | 1.0 | 1.0 | ||
| M | 3.03 | 0.007 | 2.27 | 0.006 | |
| HCT-CI scores | 0 | 1.0 | 1.0 | ||
| 1–2 | 2.56 | 1.78 | |||
| ≥3 | 3.85 | 0.001 | 2.44 | 0.005 | |
| Diagnoses | NHL | 1.0 | 1.0 | ||
| HD | 0.79 | 0.98 | |||
| CLL | 0.55 | 0.3 | 0.46 | 0.03 | |
| Graft | G-PBMC | 1.0 | 1.0 | ||
| Marrow | 0.23 | 0.03 | 0.38 | 0.03 | |
| Age, years | <50 | 1.0 | 1.0 | ||
| ≥50 | 2.72 | 0.01 | 1.53 | 0.14 | |
| Prior regimens | 1–2 | 1.0 | 1.0 | ||
| 3–5 | 2.02 | 1.71 | |||
| ≥6 | 0.79 | 0.02 | 1.44 | 0.24 | |
Figure:
2 year NRM among pts with HCT-CI scores of ≥1
Disclosures: Total body irradiation, fludarabine, busulfan, and cyclophosphamide are used off-label as conditioning agents for allogeneic hematopoietic cell transplantation.
Author notes
*
Corresponding author
2006, The American Society of Hematology
2006