Abstract
In an emerging paradigm of sickle cell disease (SCD) vasculopathy, the risk for pulmonary and systemic hypertension, renal dysfunction, proteinuria, stroke and early death may be related to the degree of hemolysis, nitric oxide scavenging and resultant damage to the vasculature (
We hypothesized that in contrast to otherwise healthy individuals without SCD, systolic blood pressures (sBP) of 120 to 139 mm Hg define relative hypertension in SCD and identify patients at increased risk for vasculopathy and its complications. We analyzed entry data from 195 adult patients enrolled in the prospective Sickle Cell Pulmonary Hypertension Screening Study (
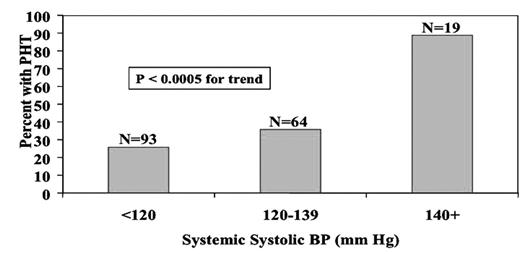
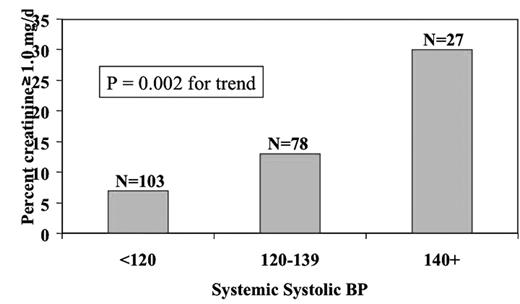
As shown in Figure 1, among Hb SS and S beta thal patients, the prevalence of pulmonary hypertension (PHTN, TRV 2.5 m/sec or greater) was 26% with sBP <120 mm Hg, 36% with sBP 120–139 mm Hg and 89% with sBP 140 mm Hg or higher (P <0.0005 for trend). Similarly, the prevalence of a serum creatinine concentration of 1.0 mg/dL or higher was 7% with sBP <120 mm Hg, 13% with sBP 120–139 mm Hg and 30% with sBP 140 mm Hg or higher (P = 0.002 for trend, Figure 2). The increasing prevalences of PHTN and renal dysfunction with the three progressively higher sBP categories are consistent with our hypothesis that sBP 120–139 represents relative hypertension and increased risk for vascular complications in patients with SCD. Whether treatment of relative hypertension in sickle patients would improve vasculopathy and lower their risk for PHTN, renal impairment or other complications such as stroke, is unknown. Consideration should be given to clinical trials to answer this important question.