Abstract
<Introduction> HPS are rare but often-fatal conditions characterized by an inappropriate and sustained activation of the cellular immune system leading to accumulation of activated macrophages and a cytokine storm. HPS consists of primary and secondary Hemophagocytic Lymphohistiocytosis (HLH). Secondary HLH occurs at any age and the genetic contribution remains uncertain. Clinical features in patients with HLH are fever, cytopenias, liver dysfunction, hepato-splenomegaly, and the presence of hemophagocytosis in the bone marrow as well as other reticuloendothelical tissues. We will report on the hematological abnormalities and the clinical course of 20/152 patients who received RI-CBT and developed secondary HLH in adult patients with hematological disease in early phase after RI-CBT.
<Object> The 1st purpose was to investigate the incidence of HLH and pattern of chimerism. The 2nd was to identify the risk factors after UCBT.
<Patients and Methods> We reviewed medical records of 152 patients with hematological diseases who had received RI-CBT between January 2002 and April 2005 at Toranomon Hospital, Tokyo, Japan. Diagnosis of HLH was made with the followings; high fever, cytopenias, and hemophagocytic findings in bone marrow examination. Time to event curves were plotted by using the actuarial method of Kaplan-Meier, and differences between curves were analyzed by log-rank tests. The following factors were considered potential predictors of outcomes about 2nd purpose: patient’s age, HLA disparity, infused TNC dose/CD34 dose, disease/disease status at transplantation, GVHD prophylaxis and sepsis which coincided with HLH. All factors were tested for the proportional hazards assumption.
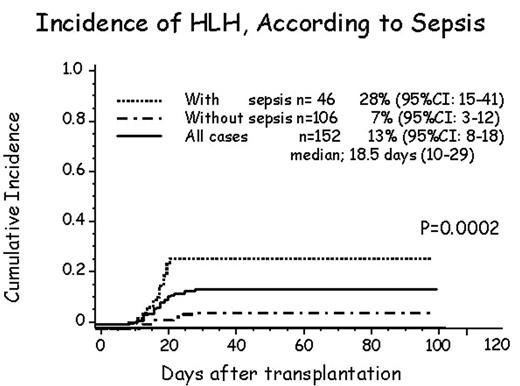
<Results> Patient’s median age was 55 years (17–79), Primary diseases consisted of standard (n=31) and advanced (n=121). HLA disparities were 4/6 match (n=123), 5/6 (n=22), and others (n=7). Total nucleated cell/CD34 cell dose were 3.46×10E7/kg (1.6–5.2) and 0.78×10E5/kg (0.1–3.3), respectively. Main conditioning regimen was Fludarabine (125mg/m2) +Melphalan (80mg/m2) or Busulfan (8mg/kg) +TBI 4Gy with cyclospoline (n=89) and tacrolimus (n=63) as GVHD prophylaxis and received single cord blood unit. Twenty patients were diagnosis with HLH and the incidence of HLH was 13% (95%CI; 8–18) and median onset day was 18.5 days (range; 10–29). In patients with sepsis (n=46) and without sepsis (n=106), the incidence of HLH was 28% (95%CI; 15–41) and 7% (95%CI; 3–12), respectively (P<0.0002). All patients who were diagnosis with HLH using bone marrow examination achieved 100% of donor chimerism. In multivariate analysis, the most important risk factor of HLH after RI-CBT was sepsis which coincided with HLH at the same times (p<0.05), while other factors did not influence.
<Discussion/Conclusion> HLH is fatal complication after allogeneic peripheral stem cell and unrelated bone marrow transplantation. However in RI-CBT, the incidence would be higher and earlier onset than other sources. The most of HLH patients died by multi-organ failure. In this report the most important risk factor was sepsis which coincided with HLH.
Author notes
Corresponding author